QME Spine Surgery Psychological Screeningby William W. Deardorff, Ph.D, ABPP, Theodore B. Goldstein, M.D., FACS.
Course content © Copyright 2014 - 2024 by William W. Deardorff, Ph.D, ABPP, Theodore B. Goldstein, M.D., FACS. All rights reserved. |
PLEASE LOG IN TO VIEW OR TAKE THIS TEST
This test is only active if you are successfully logged in.
|
IMPORTANT NOTE: This course is approved for California Qualified Medical Evaluator (QME) continuing education credits as well as other accreditations held by BehavioralHealthCE.com. If you do not need California QME continuing education credits, you should take the other Spine Surgery Psychological Screening Course. This course addresses Spine Surgery Screening as well as information specific to practicing as a QME in the State of California. In My Account, be sure to add QME to your Degree list and your QME Provider Number to your Licenses. All Degrees and Licenses will be printed on the CE certificate. COURSE OUTLINE
Introduction Learning Objectives The Back Pain and Surgery Problem Who Should Undergo Pre-surgical Screening and Why do it? Clinical Instinct: Don’t rely on it The Structure of the Spine Diagnostic Tests History and Physical Examination Imaging Studies The Problem with Imaging Studies Plain X-Ray MRI CT Scan Myelography Discogram Overview of the Test Standardizing the Procedure Interpreting the Results Confounding Factors Bone Scan Electrodiagnostic Studies Diagnoses The Purpose of Diagnosis The Reasons for Incorrect Diagnosis Various Diagnoses in Back Pain Different Types of Spine Surgery Microsurgical Discectomy Laminectomy Spinal Fusion Motion Preserving Surgeries Pre-Surgical Screening Purpose Biologic-Lifestyle Variables Work-Related Variables Psychological Factors Medical Variables Adverse Clinical Features Summary of Pre-Surgical Screening Variables Case Example Conclusion References
INTRODUCTION
This course will review pre-surgical biopsychosocial screening (pre-surgical screening: PSS) prior to spine surgery. The course will include background information about the incidence of back pain and the problem with spine surgery outcomes. The course will provide an overview of spinal anatomy, diagnostic tests, and the latest surgical techniques to treat back pain. The course will then review the most important biopsychosocial variables that are predictive of a spine surgery clinical failure. The course will present different models of PSS and provide example evaluation reports for various case scenarios:
• cleared for surgery, • cleared for surgery after preparation for surgery intervention, • cleared for surgery with pre-operative contingencies and/or recommendations, • not cleared for surgery from a psychosocial perspective and alternative treatment recommended (such as a multidisciplinary pain program).
The goal of the course is to make the practitioner comfortable with the process of completing a PSS. The information in this course is important not only for those professionals that might be completing these evaluations, but for any person involved in the care of a patient with back pain problems.
LEARNING OBJECTIVES
• Explain the process of pre-surgical screening • List the four groups of pre-surgical screening variables • Discuss problems with imaging studies relative to spine surgery decision making • Describe three types of spine surgery • Outline a pre-surgical screening evaluation report format
THE BACK PAIN AND SURGERY PROBLEM
The Back Pain Problem
It is estimated that 80-85% of the US population will experience low back pain (LBP) at some point in their lives, with a projected overall economic toll of nearly $171 billion (LaCaille et al., 2007). The costs associated with medical treatment of LBP are estimated to range from $9,000 to $19,000 per person annually (Luo et al., 2004). Workplace injuries and compensation claims are a significant aspect of these costs and are estimated at $11 billion annually in workers compensation (WC) benefits for work-related LBP and disability (LaCaille et al., 2007). A long-standing ratio has found that LBP injury constitutes 10% to 19% of all work injury claims but accounts for 33% to 41% of the total costs. Another finding is that, of the LBP work injury cases, approximately 10% of the cases account for 90% of the costs within that group. Approximately 5% of patients with acute low back pain do not respond to conservative treatment and experience chronic pain and disability (DeBarard et al., 2001). Many of these patients, particularly injured workers, seek spine surgery intervention as a treatment option. Even though it has been asserted that spine surgery is being used more judiciously, the data indicate the rate of spine surgery has steadily increased in recent decades (Deyo, 2004). Deyo reports that the annual number of spinal fusion operations rose by 77% from 1996 to 2001. In contrast, hip replacement surgery increase by 13-14% during the same time period. Approximately 300,000 patients with chronic LBP (2004 data) undergo spinal fusion surgery each year and this accounts for $16 billion in hospital charges (Deyo, 2007). It is assumed that spinal fusion will resolve vertebral instability (or movement) and consequently reduce the pain and disability. As we will see, this has not proven to be the case with many patients. Laminectomy and disc excision of intervertebral disks, aimed at decompressing nerve roots, added another $5 billion in hospital charges associated with 242,000 procedures. These figures do not include spine surgeries done on an outpatient basis, which accounts for up to 25% of procedures. The Back Surgery Problem
Spine surgery can be generally divided into two categories: medically necessary and elective. Spine surgeries that might be considered medically necessary can be found in Table 1. The results of these surgeries tend to not be influenced by non-physical factors. Elective spine surgeries (about 99% of all cases) are usually directed at relief of pain and improvement in function.
Many elective spine surgeries are quite successful, especially related to a lumbar disc herniation. Even though a majority of patients recover from this condition without surgery, some pursue surgical intervention if symptoms persist and do not respond to conservative measures. Technological advances have likely contributed to the success of surgically treating a lumbar disc herniation including: imaging techniques; improved lighting, magnification, and specialized surgical instruments and operating tables; and less traumatic dissection (Carragee, 2001). All of these advancements mean much less tissue damage associated with the surgery.
Carragee (2001) reported on 152 consecutive working patients who underwent limited open discectomy for herniated lumbar intervertebral discs. The patients were treated postoperatively with no activity restrictions and they were encouraged to return to full activities as soon as possible. At a mean follow-up of 5 years, 149 of 152 patients (98%) returned to work. The average work loss time was 1.2 weeks and 148 of 149 patients had returned to full duty within 8 weeks of the operation. Approximately one third of the group returned to work within one week of the surgery. Early return to work was not found to be associated with recurrent sciatica, reoperation for re-herniation, or ultimate clinical outcome. In another example, Zahwari (1994) treated 103 patients with microdiscectomy as outpatients. At a mean follow-up of 34.6 months, “excellent” results were achieved, including returned to work rates. Stambough (1997) reported on 175 discectomy patients treated with post-operative aggressive physical therapy. Of the group, 135 patients (77%) return to their previous work level with a mean return to work time of 6 weeks. Overall, lumbar discectomy (open, micro, minimally invasive) for sciatica has a reported improvement and success rate of between 80 and 90% (See Dubois et al., 2010, for a review).
Unfortunately, more extensive elective spine surgeries (especially within the work injury population), have not produced this type of success. More extensive spine surgeries generally include some type of spinal fusion (anterior, posterior, anteroposterior) designed to remove any movement between targeted vertebral levels. New, “motion-preserving” techniques (e.g. artificial disc replacement; ADR) also fall into the more extensive spine surgery category. Although extensive outcome data for ADR surgery in the work injured population is not yet available, there is no indication that this new technology has improved clinical outcomes over fusion.
In a meta-analytic study, Turner et al (1992) reviewed 47 spinal fusion studies published from 1966 to 1991. It was found that the percentage of patients with satisfactory outcomes varied from 16% to 95% with an average of 68%. In 56% of patients, their overall quality of life was no better or worse than before surgery, as measured at 2-year follow-up. In another study LaCaille et al. (2005) examined the outcomes associated with interbody cage lumbar fusion (ICLF). In ICLF, a “cage” (a porous cylindrical device) is placed in between the vertebra to promote fusion. It was found that, “…a considerable number of patients continued to report poor quality of life and continued functional impairment, with 38% totally disabled at follow-up an average of 2.5 years postsurgery” (p. 267). The odds of total disability were 9.1 times greater for patients involved in litigation at the time of surgery.
In another study of injured workers, DeBerard et al. (2001) assessed the outcomes of 185 injured workers who underwent posterolateral spinal fusion at approximately 5 years post-operative. It was found that 25% of the patients were totally and permanently disabled at follow-up. A total of 24% of the patients had undergone reoperation since the initial fusion surgery. A total of 41% felt that their overall quality of life had not improved or was worse as a result of the lumbar fusion (It is interesting that this figure is fairly consistent with the 68% of patient reporting “satisfactory” outcomes in the Turner et al meta-analytic study. Given statistical error, one might speculate a 60-70% satisfaction rate and a 30-40% dissatisfaction rate with spinal fusion taking into account these two studies). In the DeBerard et al. (2001) study a non-fusion rate of 26% was found. Non-fusion or “pseudoarthrosis” occurs when the bone graft between the vertebrae does not result in a solid fusion (more on this later). As has been found in other studies, correlation between solid fusion (in 74% of patients) did not correlate with other patient outcomes (r = 0.19). This data suggests that obtaining a solid fusion (“technical” success) is not an indicator of “clinical” success. Other Determinants of Spine Surgery Outcome
In seminar presentations, Dr. Goldstein will often use the quote, “There is no medical condition that cannot be made worse by surgery”, and this certainly holds true in the area of spine. Even though technological advances in the area of spine surgery have been significant, numerous patients will undergo spine surgery for chronic low back or neck pain without benefit, or even become worse. Several studies have demonstrated that purely “structural” issues (e.g. pre-operative diagnostic severity, success of arthrodesis or fusion) are not highly correlated with clinical outcomes and technical failure rarely explains a diminished surgery result; rather, poor patient selection due to psychosocial variables appears paramount. A number of psychosocial variables have been found to be predictors of clinical and functional outcome to spine surgery especially for chronic pain conditions (See Table 2).
However, there are few unequivocal predictors and these often explain a relatively low proportion of the variance in outcome. To address this problem, biopsychosocial decision-making algorithms have been developed that take into account multiple predictor variables including demographic, lifestyle, biological, work, psychosocial, and medical factors. Comprehensive pre-surgical biopsychosocial screening prior to spine surgery is an extensive process usually completed by a psychologist with special expertise in this area. Not every patient undergoing elective spine surgery is appropriate to undergo pre-surgical screening. Methods for selecting screening patients are discussed in the next section. Who Should Undergo Pre-surgical Screening and Why do it?
A failed spine surgery generally refers to a lack of clinical success including such things as decreased pain, improved function, improved quality of life and relationships, decreased need for medication, increased productivity, etc. A patient doesn’t really care that the surgeon achieved “perfect” placement of the spinal instrumentation along with a solid fusion if the clinical aspects of the problems are not improved. The consequences of a clinical failure are generally summarized under the rubric of a “failed spine surgery syndrome” (FSSS). Some of the consequences of a failed spine surgery (again from a clinical perspective) can be found in Table 3.
A patient’s appropriateness to undergo presurgical screening can be conceptualized as being on a continuum from not necessary to critical. As pointed out by Carragee et al. (2001), conditions such as metastatic cancer to the spine or idiopathic scoliosis progression are unlikely to have a significant psychosocial component affecting surgical outcome and psychological screening is not necessary. On the other hand, a disabled, work-injured, chronic low back pain patient with depression, other psychosocial issues, and equivocal structural findings, should certainly undergo pre-surgical screening. Between these two extremes, the need for the screening becomes less clear. The predictive power of pre-surgical screening in patients undergoing surgery for straightforward conditions such as a lumbar disc herniation has not been established and is likely weak (Carragee et al., 2001; Hobby et al., 2001). In this patient population, although psychological distress may be present pre-operatively, it often decreases post-operatively presumably due to the fact that the nociceptive input has been successfully remedied (See Table 4).
Clinical instinct: don’t rely on it. As discussed by Daubs et al. (2008), a majority of spine specialists do not use validated patient questionnaires to assess psychological distress; rather, they rely on their clinical instincts. Daubs et al. (2008) tested this practice by comparing a group of spine specialists’ (4 surgeons and 4 physiatrists) clinical instincts to a well-validated brief measure of psychological distress (the Distress Risk and Assessment Method, DRAM, to be discussed later). Four hundred patients presenting to a University Spine Center for initial consultation first completed the DRAM questionnaire and then were evaluated by the spine specialist. The physicians were blind to the results of the DRAM. The spine specialists were asked to place each patient in one of 4 categories: Normal, At-Risk, Distressed-Depressed, or Distressed-Somatic (these correspond to DRAM categories). According to the DRAM, the following results were found in terms of patient classification: Normal (37%), AR (42%), DD (13%) and DS (9%). As a group, physicians classified patients correctly 44% of the time. Results were better if the Normal-AR and DD-DS groups were collapsed (basically into just two groups that might be conceptualized at not significant distress and significant distress). When this was done, the physicians were correct 77% of the time. The non-operating spine specialists (physiatrists) were better than the surgeons in identifying those patients ending up in the DD-DS group. Physiatrists were correct 42% of the time and surgeons just 20% of the time. These results really underscore two issues. First, clinical judgment is not as accurate as validated objective measures and this is consistent throughout the psychometric research literature. Second, and not emphasized in the study, a total of 22% of patients fell into a psychologically distressed category (DD or DS). As will be discussed when we review the DRAM as a pre-surgical screening measure, patients in these classification groups are more likely to have a poorer clinical outcome to spine surgery.
In contrast to the situation discussed previously relative to “clean” surgical decision-making (e.g. clear findings on physical examination and imaging studies along with a condition readily amenable to surgical intervention such as a disc herniation causing sciatica), there are many cases in which pre-surgical screening is certainly indicated. Unfortunately, these cases are often identified only after a Failed Back Surgery Syndrome (FBSS) has been created. In clinical practice, most spine surgeons do not routinely use any type of pre-surgical screening or they rely on clinical judgment. If relying on clinical judgment, more comprehensive pre-surgical screening may be recommended in only the most blatant cases. These usually include severe depression or significant drug abuse.
To help the spine surgeon identify cases that are appropriate for presurgical screening, Block, Gatchel, Deardorff, and Guyer (2003) have suggested the following guidelines (See Table 5).
Based upon the Daubes et al. (2008) study, something like the DRAM might be used as a more objective screening measure for psychological distress. Deardorff (2010) has taken various components of a pre-surgical screening evaluation and distilled them into an easily implemented checklist and patient questionnaire that might be used in the spine surgeon’s office. The Brief Pre-surgical Screening (BPSS) can be used by the spine specialist to identify patients that should undergo more extensive screening (See Table 6). The variables listed in the BPSS will be discussed in greater detail subsequently. Each of these variables has been found in the evidence-based research to have some predictive power relative to spine surgery outcome. When all of these variables are considered together as part of an initial brief screening, the surgeon has a powerful tool in determining which patients should be referred for a full biopsychosocial assessment and which might be considered “cleared” for surgery from a psychosocial perspective.
What Predictor Variables Should be Evaluated as Part of a Brief Assessment?
A brief presurgical screening should assess the strongest of variables that (1) have consistently been shown to be predictive of poor spine surgery outcome and (2) are easily assessed within the context of a spine surgery practice. Lengthy pre-surgical screening procedures (e.g. interview, record review and psychological testing) are more appropriately done by the psychologist upon referral from the surgeon once the patient has been identified by the initial checklist (Block et al., 2003) or BPSS. In designing a BPSS, the most important variables from each of the four major predictor categories are assessed (See Table 2). This type of rapid assessment is easily completed in the spine surgeon’s office. Cut-off criteria can be established individually for a surgical practice depending on the patient population (e.g. workers compensation, private insurance, type of spine surgeries performed, etc.).
Any practitioner involved in presurgical screening should have knowledge of spinal anatomy, diagnostic testing related to spine surgery decision-making, and common spine surgery procedures. This background is essential when completing a biopsychosocial evaluation of a patient prior to elective spine surgery.
THE STRUCTURE OF THE SPINE
The structures associated with the spine can be divided into the spinal column, the vertebrae, the discs, the facet joints, the ligaments, the spinal canal, the sacrum and coccyx, the sacroilliac joints, the nerves, and the muscles. The Spinal Column
As can be seen in Figure 1, the back is divided into three natural curves that form an S-shape.
· The cervical curve which is made up of the bones of the neck · The thoracic curve which is made up of the middle back · The lumbar curve which is made up of the lower back
As can be seen from the side, the back is actually S-shaped as a result of these three natural curves. When the spine curves “into” the body (convex anterior) it is termed “lordosis” and when it curves “out” of the body (concave anterior) it is termed “kyphosis”. Figure 1: The curves and bones of the spine
The spine is made up of vertebra (See Figures 3 and 4), which are the bones of the spine. There are a total of 24 vertebrae in the back. The vertebrae are connected together by ligaments and muscles to form the spinal column. Aside from providing structural support for the body, the spinal column contains and protects the spinal cord. The spinal cord is the neurologic pathway for sending and receiving signals to and from the brain to the rest of the body.
Cervical spine. There are seven vertebrae in the cervical part of the spine. The cervical vertebrae support the weight of the head and protect the nerves that come from the brain to the rest of the body. These vertebrae are referred to as C1 through C7, with C1 being the vertebra just under the head. The natural curve of the cervical spine is “inwards” (lordosis). The first cervical vertebra (C1) is unique in that it is a ring that rotates around the second vertebra (C2). Most rotation of the neck (moving the head from side to side) takes place in the first two segments C1 (also called the “atlas”) and C2 (also called the “axis”). Flexion (moving the head forward) and extension (moving the head backward) are mostly controlled by C5-C6 and C6-C7. Thoracic spine. There are 12 vertebrae in the thoracic part of the spine which is the mid-back. These are referred to as T1 to T12, with T-12 being at the lower end. The thoracic spine is firmly attached to the rib cage and sternum (breastbone) and, relative to the cervical and lumbar areas, does not have much motion. Consequently, the thoracic spine is the site of the least amount of elective spine surgery. The natural curve of the thoracic spine is “outwards” (kyphosis).
Lumbar spine. There are usually five vertebrae in the lower back, referred to as the lumbar spine. These are referred to as L1 through L5. However, some people have a sixth lumbar vertebra and you will occasionally see an L6. The vertebral arches (see Figure 5, made up of the lamina and pedicle) are connected by paired facet joints. In combination with the disc this creates a three joint complex at each functional unit. This three-joint complex at each functional unit allows for motion in flexion, extension, rotation, and lateral bending. This three joint complex is where most spine surgery is directed.
The vertebrae of the lumbar spine are very large in construction since they must carry the weight of the other parts of the spine. The normal curve of the lumbar spine is “inwards” (lumbar lordosis). The lumbar curve is the workhorse of the spine and motion includes “flexion” (moving forward), “extension” (moving backward), moderate lateral flexion (sidebending), and a small degree of rotation. It is the part of the spine that carries the majority of weight and moves the most. When bending forward (flexion), 50% percent of the motion occurs at the hips and 50% occurs at the lower spine (lumbar). Of the motion that occurs in the lumbar spine, most is in the lower segments, L3-4 and L4-5. The two lowest discs (L4-5 and L5-S1) take most of the strain of the lumbar spine and are where most back problem occurs.
Given the unique demands on the lumbar spine, surgical technology has focused on developing “motion-preserving” procedures such as the artificial disc replacement (ADR). In contrast to a lumbar fusion which removes the motion between two vertebrae by fusing them together, motion-preserving techniques seek to maintain natural movement. We will discuss this further under types of spine surgeries. The lumbar spine is the area where the vast majority of spine surgery occurs. Figure 2: The sacrum and coccyx
Sacrum. The base of the spine, called the sacrum, is a group of specialized vertebrae that connects the spine to the pelvis (See Figure 2). The sacrum is composed of five sections (called S1 to S5) that are fused into a single bone called the sacrum. When one of the upper bones forms as a vertebrae rather than a part of the sacrum, it is call a transitional (or sixth; L6) vertebrae. This occurrence is not dangerous and does not appear to have any adverse effects. The uppermost vertebra of the sacrum is referred to as S1. In spine problems, you will often hear about the L5-S1 area.
Coccyx. The coccyx is made up of between 3 and 5 vertebrae, usually counted as 4 bones. The vertebrae are actually fused together and are collectively known as the coccyx or “tailbone”.
The sacroiliac joints. The sacroiliac joints are the joints that attach the sacrum to the iliac bones of the pelvis (see Figure 2). If you place your hands on your hips, you are feeling your iliac bones. Although it has previously been thought that this joint could become misaligned and cause pain, this issue remains controversial. It is unknown how much pain is actually generated by the sacroiliac joint, and if it actually can become misaligned. Figure 3: Vertebra, side view
The Vertebrae
The vertebra (plural: vertebrae) are the bones of the spine. The vertebra has three parts:
· The vertebral body · The transverse process · The spinous process Figure 4: Vertebra, top view
Figure 3 shows a view of a vertebra from the side and Figure 4 shows it from the top. Figure 4 shows a view of two vertebrae with a disc in between. The vertebral body is the large part that surrounds and protects the spinal cord. The spinous process is the part of the vertebrae that can be felt as the bony bumps on the back. The transverse process provides an area of attachment for muscles that control movement of the spine. Other structures that will be important to remember when we discuss various types of back surgery include the lamina and the pedicles. For instance, a “laminectomy”, which is a component of many spine surgeries, involves removing the lamina to gain access to the spinal canal. Spinal fusions using instrumentation include the use of pedicle screws and these are anchored into the pedicle bone of the vertebrae. Also notice the opening through which the spinal cord passes which is termed the spinal canal or vertebral foramen (literally “opening”). Figure 5: A functional unit The Discs
The discs (or “intervertebral discs”) are the cushioning pads or “shock absorbers” of the spine. The discs lie in between each of the vertebrae (See Figures 4 and 5). Figure 4 shows two vertebrae with a disc in between. These three parts (two vertebrae and a disc) are also known as a “functional unit”. Figure 6 shows a cut-away view of a functional unit. In general, the intervertebral disc has three important functions (See Table 7):
As can be seen in Figure 6, the disc is made up of two parts: The central portion with a gelatin-like consistency called the “nucleus pulposus”. The nucleus pulposus is actually a loose network of fibers suspended in a mucoprotein gel. This spongy center provides nourishment, lubrication, and shock absorption. A healthy intervertebral disc contains a great deal of water in the nucleus pulposus and this gives it the spongy quality allowing it to absorb spinal stress. At birth, the nucleus is made up of 80% water. The nucleus relies on its water content to maintain strength and pliability. As we age, the spinal discs dehydrate and become less pliable and less able to adjust to compression. In the vast majority of cases, this does not cause pain.
The tough outer layer is called the “annulus fibrosus” (or “fibrous ring”) and is composed of concentric sheets of collagen fibers (lamellae) that surround the inner core. The annular fibers hydraulically seal the gelatinous nucleus and evenly distribute pressure and force imposed on the functional unit. The annulus fibrosus attaches to the vertebrae holding them together. The design of the disc allows the bony vertebrae to move back and forth, giving the spine great flexibility.
Pressure on the nucleus pulposus is 5 to 15 times greater than blood pressure and blood does not reach the nucleus. Since the nucleus does not have a blood supply, the disc does not have a way to readily repair itself after damage and the pain created by a damaged disc can last for quite some time. There are no nerve endings in the nucleus but they are located in the most external layers of the fibrous ring. This explains why disc degeneration (as occurs with aging) may not be painful if the external layers of the fibrous ring are not affected. Figure 6: The three parts of the disc
The Facet Joints
Between each vertebrae there is a gliding joint called a facet joint which can also be seen in Figure 7. Facet joints help keep the vertebrae aligned as the spine moves. The facet joints are held together by ligaments called joint capsules, which consist of a smooth lining called synovium. The synovium produces synovial fluid in the joint capsule and this helps lubricate the joint for smooth movement while also providing nourishment. The facet joint capsules have a supply of tiny nerve fibers that can cause pain if irritated.
The Ligaments
As can be seen in Figure 7, there are a number of ligaments that “knit” the spine together and also contained pain fibers. For the purposes of our discussion, we will focus on only two:
· The anterior (toward the front) longitudinal ligament · The posterior (toward the rear) longitudinal ligament
These ligaments connect the functional units (2 vertebrae and a disc in between) together and go up and down the entire length of the spine. These ligaments help control the motion of the spine while also providing flexibility.
Figure 7: The ligaments of the spine
The Spinal Canal
The spinal canal can be seen in Figure 5. It is the opening that is formed by the vertebrae since they are aligned on top of one another. The spinal cord passes through this opening and is well protected by the bony vertebrae. It is a tube that is partly filled with a fluid called cerebral spinal fluid (CSF). This is the same fluid that is in the center part of the brain. CSF helps protect the spinal cord within the spinal canal. The Nerves
The spinal cord is made up of nerves which extended from the brain into the spinal canal and then out to the various parts of the body. The spinal cord runs throughout the cervical and thoracic spine and ends at the lower part of the thoracic spine. The spinal cord does not run through the lumbar spine. After the spinal cord stops at the lower thoracic level, the nerve roots from the lumbar and sacral levels spread out like a “horse tail” (cauda equina) and exit the spine. Because the lumbar spine has no spinal cord and there is a lot of space for the nerve roots, serious conditions such as paraplegia due to a disc herniation are unlikely.
The spinal cord can be divided into segments according to the nerve roots that branch off of it: 8 cervical nerves, 12 thoracic nerves, 5 lumbar nerves, 5 sacral nerves and 1 coccygeal nerve. Lumbar spine nerve roots are named for the upper segment from which it emerges (e.g. the L4 nerve root is at L4-L5). Figure 8: The spinal cord, nerve roots and spinal nerve branches
Figure 8 shows the nerve roots at various places along the spine. As can be seen, the nerves exit the spinal cord at different points and go out the various parts of the body. Figure 8 shows a close up view of the spinal cord, nerve roots and the spinal nerve branches. The most common nerve pain problem results from a disc bulge or herniation. This occurs since the nerve root runs over a relatively weak spot in disc space which is more likely to “bulge” or herniate. In this condition, part of the disc bulges or “herniates” out of its usual space and ends up pressing on one or more nerves. This pressure on the nerve root often causes pain down the arms if it occurs in the neck area and pain down the legs if it occurs in the lower back (called “sciatica” since the pressure is on the sciatic nerve).
The Muscles
There are a great many muscles involved in the function of the spine. These include those in the back area as well as the abdominal area. For the purposes of this discussion, we will only review the most important muscles involved in spine function and back pain problems.
The erector spinae muscles are on either side of the lower spine. When discussing muscle spasms in the back, it is these muscles that are the culprits. Just under these long muscles are medium length muscles that extend from one vertebra to the next. There are even shorter muscles underneath these that attach to the facet joints. All of the muscles discussed thus far are in the back area. Moving to the side and front part of the body, there is another important muscle called the “psoas muscle”. It runs from the front and sides of the lower back, across the hip joint, and attaches to the very upper part of the thighbone (femur). Moving completely around to the front of the body, there are the important abdominal muscles. These muscles are critical to the forward movement of the spine, as well as providing support. This is why in physical therapy the patient will often be instructed to focus on strengthening the abdominal muscles as part of a back pain rehabilitation program (“core strengthening”).
DIAGNOSTIC TESTS
In recent years there has been an explosion in high technology approaches to assessing back pain. These include such things as the CT scan and MRI, both of which we will discuss in this section. Even with these tests, the most important “test” is the history of the back pain problem and the physical examination. In addition, being aware of the usefulness of psychological assessment of back pain is essential.
The History and Physical Examination
The most important diagnostic test with respect to a patient’s back pain is a complete and thorough history taken by the spine specialist in a face-to-face interview. The history of the back pain problem should be done in conjunction with a physical examination. A healthcare practitioner who is well-trained in spinal disorders should have a relatively clear idea of what is causing the back pain after the history and physical. The physical examination should be done to confirm the diagnostic impressions based on the history. To get a good idea of a back pain problem, the healthcare practitioner should assess both physical and emotional issues. As we discuss throughout this course, it is extremely important to do an assessment of the entire person, including the mind and the body. A component of the pre-surgical screening is to assess how well the patient has been physically evaluated by the spine specialist and how these findings have been correlated with the other diagnostic study results. IMAGING STUDIES
The Problem with Imaging Studies
If the doctor focuses only on the structural diagnostic possibilities, the diagnosis and treatment will often be incomplete and incorrect. Unfortunately, advances in technology over the past several years have given doctors the impression that they do not need to rely as much on a good history and physical examination. They simply proceed to the diagnostic testing for the answer as to the “cause” of the low back pain. Patients are often very willing to accept this approach because they believe the high-tech machines are more accurate and more "scientific". Nothing could be further from the truth. These tests, such as the MRI and CT scan, are very sensitive and allow doctors to see normal wear-and-tear changes in the spine that were previously not observable. Unfortunately, as we have discussed, many doctors interpret these normal changes as being "abnormal" and proceed with scary sounding diagnoses, inappropriate recommendations and treatments, and surgery.
It is more critical than ever that the history and physical examination be detailed and appropriate so that the doctor can identify those changes seen on the high-tech studies that are clinically significant and those that are not.
Plain x-rays
When used to assess back pain, x-rays allow for visualization of the bones of the spine, sacroiliac joint, and pelvis. An x-ray can identify whether or not there are changes associated with normal aging, fractures, and overall alignment of the spine (scoliosis). X-rays may be appropriate when:
lower back pain that has not resolved over the initial two or three weeks of conservative treatment in a person who has back pain even during periods of no activity
when there is back pain that awakens the person from sleep at night
The decision to obtain an x-ray, or any other test, should be guided by the history and physical examination. Supposedly “abnormal” findings on the x-ray generally are not significant. In fact, in many cases they will not relate to the back pain that the patient is experiencing. Positive findings which might relate to back pain include such conditions as a fracture, severe degeneration, or significant scoliosis. A negative x-ray is not uncommon in back pain cases since a great majority of painful back conditions come from the soft tissues of the spine including the muscles, joint capsules, tendons, and ligaments. None of these structures can be seen on x-ray.
An x-ray test should not routinely be used on a person’s first visit to the doctor for back pain unless there are very clear reasons (e.g. the possibility of a fracture due to trauma). Although an x-ray is often obtained on the first visit to the doctor for back pain, it has been shown to generally not be worthwhile. In a recent study of primary care patients with low back pain, obtaining lumbar x-rays prior to treatment was not associated with improved function, reduced pain or improved health status after treatment (Kendrick et al., 2001). Participants receiving x-rays were more satisfied with their care but were not less worried or more reassured about serious disease causing their low back pain. Ironically, patients receiving x-rays, although more satisfied, demonstrated more doctor visits and more disability three months later. This underscores the fact that ordering diagnostic tests is not a benign process relative to the treatment outcome. Completing a test when it may not be necessary (or to serve some other need such as defensive medical practice), can communicate a powerful message to the patient that may impede response to treatment. The MRI (Magnetic Resonance Imaging)
MRI uses a strong magnetic field, radio waves, and a computer to obtain a picture of many structures of the spine. The MRI does not use x-ray exposure nor does it require any exposure to radiation. The MRI shows nerves, muscles, ligaments, and discs, as well as the bones of the spine and gives much more information than x-rays. No specific risks have been found with the MRI, although it is not known to be totally safe for women in early stages of pregnancy and is not recommend for patients with implanted devices (e.g. pacemaker). MRI’s are generally appropriate if the patient:
· has not responded to appropriate conservative management over a period of 6 to 8 weeks · is being considered for interventional pain management treatments (e.g. blocks) · is a possible surgical candidate · is possibly suffering from an infection or tumor of the spine
It is not generally used in the early stages of back pain unless an infection or tumor is suspected. The MRI test is extremely sensitive and allows one to see the very subtle aging changes in the spine that should be considered to be normal in a large percentage of the population. These changes do not relate to back pain and occur in individuals without symptoms. This is especially true for the age group over 35 to 40 years old.
The MRI procedure is safe and virtually without side effects. However, approximately 20 percent of patients who undergo the procedure find being in the tube uncomfortable due to feelings of claustrophobia (“being uncomfortable in a closed space”). In some cases, an MRI will be done with an “enhancement agent”. This is a fluid that is injected into the patient’s arm or leg prior to the test. The substance can help provide an MRI picture that is much clearer, especially in patients who have had prior spine surgery. We should mention that there are "open machines" that are advertised all the time in the newspapers. These machines purport to solve the claustrophobia problem for patients. Unfortunately, the resolution and quality of the MRI picture suffers greatly in these open machines. It is best to have an MRI done in the best machine possible (this is usually a closed machine with the largest magnet). Having the MRI in the best machine will give the best results in terms of image quality.
Even with the high technology of MRI, there are still certain sources of pain that cannot be seen. This includes such things as inflammation, a sprain-strain in the muscles or ligaments, and the impact of psychological factors. Of course, as we have discussed previously, there are always the psychological and emotional influences on pain that MRI cannot assess.
The CT Scan
CT scan stands for “computerized tomography”. It is also referred to as a CAT scan which is "computerized axial tomography". These words represent the nature of the test: Computerized means that a sophisticated computer is required to make the final picture. Tomography comes from the Greek words "tomos" (which means a slice or section) and "graphia" (which means recording). Thus, a CT scan is a computerized recording of a slice or section of the body.
The CT scan uses x-ray to produce a cross-section picture of the body. There is a moderate amount of radiation exposure with a CT scan that is greater than one would experience from a plain x-ray but it is well within the safe range. The test is designed to show the anatomy of the bony structures of the spine as well as discs and nerves. The CT scan does not show the soft tissues, nerves, and muscles quite as well as the MRI. A physician might choose a CT scan over an MRI scan:
· if the patient is very claustrophobic and cannot tolerate being in the MRI machine even with the sedative · if there is a special need to see the anatomy of the bony structures where the nerves exit the spinal canal
The latter of these two reasons is only relevant to a patient that is being considered for surgery. As with the MRI, CT scans are sometimes done with a contrast agent. These agents are injected into the patient prior to the test and help make certain aspects of the picture clearer.
As with all of the other imaging studies, one must be cautious about interpreting supposed abnormal findings on the CT scan as actually being the source of an individual’s back pain. CT scan results mean nothing unless they are correlated with the history and physical examination information.
Myelography
A myelogram is an x-ray of the fluid filled sack around the spinal cord. In this test, a contrast agent or dye is injected into this sack by a radiologist to enhance the x-ray study. The myelogram is frequently followed by a CT scan, done within one or two hours after the contrast agent or dye is injected. When used in this way, the test allows the doctor to see the bones or skeletal structures as well as the neurologic structures such as the nerves. The nerves can be seen because the contrast agent or dye outlines them on the picture.
This test is generally only appropriate if surgery is being considered. One common use is in the elderly population who have spinal stenosis and the physician wants to image the spine with the person standing as well as bending forward and backward. It is also helpful in the unusual case when an MRI or CT scan is not clear and there is a question about the presence of a tumor.
Unless the patient being referred for the myelogram would consent to undergo spine surgery as a possible treatment, there is no point in undergoing this invasive test. In most cases, minimal to moderate pain is associated with the myelogram procedure. Years ago the test was done in the hospital but due to new technology and improved safety it is now done on an outpatient basis. It begins with the patient lying on a table so that the dye can be injected into the spinal canal. This takes approximately one or two minutes. The patient may feel a slight prick as the needle is inserted. Once the dye is injected, plain x-rays are taken with the patient in many positions including standing, partially upright, lying down, and turned to the right or left side. The CT scan may then be done. The entire process takes approximately one hour.
After the completion of the test the recovery period is approximately 6 to 12 hours. The patient is instructed to lie with his or her head slightly elevated and to drink plenty of fluids. This keeps the contrast material or dye away from sensitive areas in the head while flushing the material from the body. Headache is a side effect that can occur due to one of two reasons: a reaction to the dye or a spinal fluid leak. In the first situation, the reaction to the dye occurs with a frequency of less than one percent. This is because the newer dyes are water-soluble and have been introduced over the past five years. The second reason for a headache is due to a spinal fluid leak and this situation occurs in approximately 5 to 10 percent of patients undergoing the procedure. This side effect is a headache that lasts for one to two days following the test. It is due to a small amount of cerebral spinal fluid (the fluid that circulates around the brain and spinal cord) leaking out through the needle hole. This almost always subsides with a short period of rest and the intake of fluids. Discogram
The discogram test will be discussed in greater detail since it has become increasingly used as a means to evaluate patients for spine surgery. In addition, this test (specifically the “provocative discogram”) is actually significantly influenced by psychological factors. Therefore, it is most appropriate to complete a biopsychosocial pre-surgical screening before the discogram (a pre-discogram screening). The screening will assess whether psychological factors would preclude obtaining a valid discogram and address pre-surgery issues. If the patient fails the pre-discogram screening, the test should not be completed and non-surgery treatment alternatives should be explored. A discogram should only be completed if the patient is being considered for spine surgery and would choose to undergo the operation if it is recommended.
Overview of the test. A discogram is a test that involves injecting a sterile liquid (dye) into multiple discs causing pressurization designed to determine which discs might be causing the pain. (See an animated video describing the discogram procedure). Since one part of the test relies on a patient’s report of pain, it is also termed a “provocative discogram”. The patients lie on either their side or stomach on a table equipped with a fluoroscopic (x-ray) unit. The patient is placed under IV sedation; however, it is important for the patient to be alert and coherent enough to tell the physician about the pain they are experiencing. Therefore, it is important to use sufficient local anesthetic but as little general sedation as possible (to keep the patient comfortable but coherent). The physician will first infiltrate local anesthetic under the skin. Using fluoroscopy to guide the needle insertion, the physician inserts a guide needle to the outer edge of the disc; then, a smaller needle is inserted through the guide needle and into the center of the disc. This procedure is repeated for all discs that are being included in the test. Needles are usually placed in at least three consecutive levels. Once all of the needles are placed, the discs are pressurized one at a time with injections of contrast dye.
The patient is not told which disc is being done during the procedure. The patient should be unaware of the precise moment of pressurization and the level being assessed. For each pressurization, the patient (who is conscious but slightly sedated) is questioned about his or her pain. The physician is looking for disc pressurization that results in pain that is similar in quality and distribution to what the patient normally experiences. After each disc is tested, images are taken with the fluoroscopic unit and then removed. The patient may then be sent for a post-discogram CT scan. If the patient asks the physician or spine surgeon, he or she might be told that this test is mildly to moderately painful. However, most of the patients we have treated describe it as somewhat more colorful terms (words like “barbaric”, “torturous”, etc.).
Standardizing the procedure. To increase the reliability, validity, and utility of the procedure there have been attempts at standardization. This is due to the fact that a number of the components can either be done inconsistently (e.g. the amount of pressurization, telling the patient which levels are being assessed, etc) and be influenced by purely subjective factors (the patient’s report of pain intensity, patterning, etc.). Some the important elements of the discogram can be seen in Table 9.
Interpreting the results. The criteria for a positive discogram are controversial and varied, especially in the clinical settings. The diagnostic criteria for a positive discogram usually include three components:
· Significant report of pain at the suspected level (e.g 6 out of 10) · Reproduction of the patient’s typical pain in terms of quality and distribution (concordant) · No pain or minimal pain at the “control” level
Some discographers will add other criteria such as attempting to objectify the pain by assessing the patient’s facial expressions or monitoring heart (this is usually only done in an experimental setting).
Confounding factors. As review by Carragee and Don (2010) there are various confounding factors that will invalidate the results of the discogram. Although these are multiple, the most important relative to the current discussion is psychological factors. Psychological factors can increase pain sensitivity resulting in reports of pain in response to factors other than stimulation of a pain generator. Since the discogram has a significant subjective component (the patient’s report of pain), it is very susceptible to non-physical influences. Therefore, psychological screening should be done in appropriate cases prior to discography. Additional “yellow flags” relative to the discogram results include presence of a chronic pain syndrome (see the chronic pain management series), multiple positive levels, and/or a positive finding at the control level. Overview of validity and utility issues. Please see Caragee and Don (2010) for a complete review of these issues. Some of the challenges relative to discography include the following:
Block et al. (1996) found that patients with elevated MMPI scores on Scales 1 (Hypochondriasis) and 3 (Hysteria) were significantly more likely to report pain during the injections than those without the abnormal MMPI profiles. Similarly, patients who produce abnormal pain drawings have been found more likely to report increased pain reports during injection of a nondisrupted disc (Ohnmeis et al., 1995). These studies, and those similar, underscore how pain sensitivity can impact report of pain during discography.
Studies have shown that patients with minimal or no back pain will show positive results on discogram. For an extensive review see Wolfer et al. (2008). Derby et al. (1999) found that 43% of patients with minimal or occasional back pain which did not require treatment had pain ratings equal to 5 or greater out of 10 on the discogram test. Carragee et al. (2002) found that 36% of patients who had mild persistent back pain that did not require treatment had positive and concordant discograms. This group also showed annular disruption at the positive levels and negative control levels. As discussed by Carragee and Don (2010), all of these patients would have been found to have fully positive discographic results indicating discogenic pain. These tests, and others, indicate that even discs found to be positive on discography may not necessarily be pain generators. The results from studies of asymptomatic patients have been criticized on methodological grounds (See Manchikanti et al., 2009 for a review).
Bone Scan
The bone scan is a test that requires the injection of a special radioactive dye into the individual's arm. The radioactivity of the dye is extremely low and safe. After the injection, the patient lies down while the dye is allowed to circulate for about two hours throughout the entire body, including the bones of the skeleton. Once the dye has had a chance to circulate, special x-rays are taken to determine how much of the dye has penetrated into various parts of the skeleton. The scan works by detecting an increase in radioactivity in any part of the skeleton that has an increase in blood flow. The increase in blood flow can be due to either a tumor, infection, or a fracture. The bone scan is generally used when these conditions cannot be diagnosed by plain x-ray, MRI, or CT scan. In general there are no risks with the test, although some patients with back pain find it difficult to lie down for the extended period of time while the dye is circulating. As with the other tests we have discussed, the results must be interpreted as part of the entire evaluation. The most common mistake made in interpreting a bone scan is to attribute too much significance to a "finding" that is due to normal arthritic or wear-and-tear changes in the facet joints.
Electrodiagnostic Studies
The most common electrodiagnostic studies used in back pain include electromyography (EMG) and nerve conduction studies (NCS). This testing is designed to measure the electrical activity and function of nerves and muscles. The tests can show if the electrical activity of various nerves have somehow been disrupted. During the study, the physician will insert small needles into several muscles being measured. These tests can be mild to moderately painful. In an EMG, these needles are connected to a monitor that will show the electrical activity of the nerves and muscles. In a nerve conduction study the nerves being studied are "buzzed" with an electrical pulse so that the electrical activity can be monitored by special receiving electrodes. These tests can be helpful to determine a variety of diagnoses in which there may be problems with the nervous system or to assess the regrowth of nerves after lumbar disc surgery for sciatica. Electrodiagnostic studies are becoming less necessary since the majority of diagnoses in patients with back pain can be made by a good history and physical examination in addition to the other diagnostic tests available that we have discussed previously.
DIAGNOSES
If you are involved in pre-surgical screening prior to spine surgery, it is important to understand some of the common diagnoses in back pain.
The Purpose of Diagnosis
In traditional medicine the three principles of treatment are "diagnoses, diagnoses, and diagnoses." This is because it is generally thought that in medicine, if you do not know what is wrong, you cannot give proper treatment to "fix it". There are several problems with this approach in back pain: An exact anatomical diagnosis for back pain problems is rarely found. In fact, an exact diagnosis for acute back pain is possible only about 10 to 15 percent of the time. Also, treatment for back pain can be very effective without knowing the exact cause.
In most cases the physician’s job is to rule out certain diagnoses that can be serious life-threatening illnesses that need immediate attention:
· Tumors · Infections · Progressive nerve root damage · Significant spinal instability that puts the spinal cord in danger
Modern clinical examination and diagnostic techniques are very good at determining these extremely rare conditions. These techniques are also excellent at determining back pain conditions due to such things as disc herniation or spinal stenosis. Even so these modern techniques must be used very carefully as they can often lead to excessive fear in the patient as well as incorrect treatment. Once a serious condition is ruled out one is often left with back pain of an unknown origin. As we have discussed, this constitutes the vast majority of back pain cases. Keep in mind that the treatment approach can be very effective even without knowing the exact cause of the pain. It is this situation that makes back pain unique from most other conditions in medicine.
Patients often have the "need" to have some kind of diagnosis even if there is little real evidence that this diagnostic explanation is causing the pain. This need for diagnoses affects both medical and other health care approaches. Because people have a need to have a “diagnosis” and doctors are trained to give one, health care professionals of all types will comply by focusing on some anatomical variant noticed on a new imaging study or other high-tech approach and say, “that is the cause of your pain” when, in fact it has nothing to do with it. The patient would rather hear that, "your pain is due to a bulging disc or a spine that is out of alignment" versus "we don't know what is causing the pain but we can still get you better". People will be attracted to the person that says "I know what is causing your pain" even though the reality is that no one knows what is causing the pain in 85 percent of the cases. Unfortunately, this need for diagnoses can lead to incorrect and unnecessary treatment, including spine surgery. In many of these cases, the person with back pain would have improved whether or not the treatment was administered. The Reasons for Incorrect Diagnosis in Back Pain
There are three main reasons people are given incorrect diagnoses for their back pain problem: diagnosing based upon an imaging study, ignorance on the part of the health care practitioner, and lack of appreciation of psychological and emotional factors.
Diagnosing based upon an imaging scan. One of the most common reasons for being given an incorrect diagnosis is that a structural diagnosis for the back pain is made based upon an imaging scan. This process is part of the patient's need to have some kind of diagnosis and the doctor's need to give one. The doctor believes that showing the patient some type of supposed problem on an x-ray or MRI will serve this purpose even if the findings have absolutely nothing to do with the pain. What the doctor doesn't realize is that explaining these findings to the patient as being "significant" can cause the patient to believe that his or her spine is now "damaged" when in reality it is not.
Imagine how upsetting it would be for a forty-year old man with low back pain to be told that it is due to these "arthritic" changes seen on the x-ray. The patient now believes that his spine has deteriorated so much at the age of 40 that he is experiencing back pain. He also believes that "things can only get worse" even if his doctor does not explicitly make this statement. The truth is that such changes are commonly seen on x-ray in the vast majority of forty year-old men that do not have back pain. Therefore, these supposed "findings" probably have nothing to do with the person’s back pain at all. Even so, the doctor will point out the changes and state that this is the cause of the back pain simply to fulfill this need for diagnosis on the part of the patient and the doctor.
Ignorance on the part of the health care practitioner. Commonly, an incorrect anatomical diagnosis is given to a patient due to ignorance on the part of the health-care practitioner. Only recently have doctors started to appreciate the extent of asymptomatic findings (findings which do not cause symptoms) on sophisticated imaging studies such as MRI. Previously, doctors thought that any finding such as a disc bulge or herniation had to be significant. It is now known that a great number of "findings" on these tests such as disc herniations, minor scoliosis, and other radiographic abnormalities don't necessarily have any correlation to the patient symptoms. Many research studies have shown that people with no back pain or symptoms at all will show abnormalities or variance on things such as x-ray and MRI. These findings are now being understood as normal variations in the human spine and not anything significant.
Lack of appreciation of psychological and emotional factors. Most practitioners who diagnose and treat back pain do not have an appreciation for the power of psychological, emotional and social factors in back pain. We have seen how these issues can impact back pain in chapters three and four. An example of such a condition is stress related back pain in which the primary cause of the pain is thought to be emotional. Another example is chronic back pain in which psychological and social factors become extremely important to consider. If the health-care provider is not aware of these influences on back pain, the likelihood of an incorrect diagnosis along with inappropriate treatment is very great.
Diagnosis in Back Pain
In this section, we will discuss common back pain diagnoses that might lead to the recommendation to undergo spine surgery. As we have discussed, there are three rare conditions that are very serious and require aggressive medical treatment, usually including surgery. These are cauda equina syndrome, a spinal tumor, a spinal infection. These conditions can be quickly diagnosed with modern testing techniques. Herniated disc/sciatica. As discussed in the anatomy section, the discs lie between the vertebrae and act as cushions for the spine. A disc bulge or herniation occurs when the soft gel like material of the nucleus pulpolsus pushes out from between the vertebrae in one of two ways:
Bulge- (disc protrusion)-when the disc bulges out and does not actually break through the outer ring (annulus pulposus) or ligament. Bulging discs are very commonly seen on MRI's and are often not symptomatic.
Herniation-when the disc bulges toward the back of the body (posteriorly) and breaks through the annulus fibrosis (an annular tear) it is referred to as a herniation. Tears or disc herniations are almost always posterior-ipsilateral in nature owing to the presence of the posterior longitudinal ligament in the spinal canal.
A bulging disc does not usually cause any symptoms as there is no irritation or compression of nerve roots of the spine. This is supported by the following finding:
After the age of forty years old the incidence of bulging disc is seen in 50 percent or more of MRI scans in individuals without symptoms
In a herniated disc the gel like material of the nucleus pulposus can press against a nearby spinal nerve and cause pain typically referred to as sciatica. Sciatica pain occurs when the nerves of the lumbar spine are "pushed against" or compressed by a herniated disc where the nerves exit through the vertebral canal. These nerves supply the sensation and strength to the legs extending all the way down to your feet. Several important facts about disc herniation are: More than 90 percent of all herniated discs in the lumbar spine occur at the levels of L4-5 and L5-S1, with the former being more common.
Sciatica pain typically occurs in the buttocks, back of the thigh and calf, and occasionally down to the foot and heel.
The nerve root is most commonly "compressed" but not "compromised". This means that it is irritated but still works.
Occasionally, however, the nerve is so compressed that it causes a decrease in strength, sensation, and reflex. Although this condition may require surgical treatment, the great majority of disc herniations respond to nonsurgical, conservative management.
Since the use of MRI has become common, a very high incidence of herniated discs in patients without back pain or sciatica is being seen. Research has that shown that over 35 percent of individuals without symptoms over the age of 40 are found to have herniated disc on MRI. We frequently see patients who have been given a diagnosis of a herniated disk (based on MRI) and it is clear that the herniated disc that was found has absolutely nothing to do with the patient’s pain. This is a case of "the need for diagnosis" that we discussed previously. In these cases the patient has been "scared by the diagnosis" even though it is not the reason for the back pain or symptoms. Even worse is when a patient undergoes surgery for this non-offending herniated disc and his or her symptoms continue unchanged even after the operation. In this case, the patient has had an unnecessary spine surgery that does not solve the pain problem.
A herniated disc, even in the presence of nerve root compression, is very rarely a serious problem. It should only be considered serious if there is:
· a progressive weakening of the muscles of the lower extremities · a loss of sensation in the lower extremity · a cauda equina syndrome in which nerves that supply the bowel and bladder are starting not to function
In most cases the herniated disc merely causes some pain with a mild sensory loss, reflex loss, or weakness, which frequently returns as the patient recovers. The natural history of a disc herniation is very favorable with the great majority of patients showing spontaneous recovery within two to three months of conservative treatment. Even if the symptoms continue to a chronic stage (more than about three months) the patient still has the choice of continued conservative management. Ongoing pain and symptoms, in and of themselves, are not necessarily reasons to have surgery.
Pinched nerve, nerve compression, and spinal cord compression. A "pinched nerve" is a commonly used term to represent what we have discussed previously as sciatica due to irritation of a branch of the sciatica nerve. This could be due to a disc herniation or bulge, or a mechanical problem. Spinal cord compression is something that very rarely occurs since the spinal cord actually ends about four to five inches above where 95 percent of disc herniations occur. Spinal cord compression is seen in the very rare case of a disc herniation that occurs in the thoracic spine (the mid-back). As we have discussed, disc herniations are rare in the thoracic spine due to the increased stability of this part of the back provided by the rib attachments.
Arthritis of the spine. Arthritis is a general term that means “inflammation of a joint or joints” in any part of the body, including the spine. There are many different causes and types of arthritis. Some are part of the natural aging process and cause no symptoms while others can be quite severe in terms of deformation of the joints and pain. Unfortunately, most people associate the term "arthritis" with rheumatoid arthritis. This is the condition that they have seen in their grandparents or other older persons who have gnarled fingers and a crooked spine. This type of arthritis can cause pain and malformation of any joints in the body, but rarely in the spine. When this type of arthritis does occur in the spine it is a condition known as ankylosing spondilitis. This condition does cause more severe inflammation, stiffening and pain. Ankylosing spondylitis is rare and most often diagnosed by a rheumatologist. Appropriate testing for this condition includes X-ray findings of joint deformity and blood tests.
The association of the term "arthritis" with "rheumatoid arthritis" has made arthritis a very scary label. When speaking of "arthritis of the spine" doctors are most often referring to findings on x-rays and MRI that are actually part of the natural aging process and not associated with any symptoms. These findings often play absolutely no role in a person’s back pain. In reality, the term arthritis should rarely be used when discussing joint changes in the spine. All too often, doctors use it as a technical term to describe findings on imaging studies (which are actually normal) and end up scaring their patients to death for no reason. We cannot count the number of times young to middle-age patients have come to us saying, "my previous doctor told me I have the spine of an 80 year old" . This message from the doctor created great suffering and fear in these patients for no reason. Due to this, we feel the use of the term "arthritis" of the spine should really be restricted to those cases of ankylosing spondylitis or rheumatoid arthritis. Degenerative disc disease. Degenerative disc disease of the spine is not a true "disease" in most instances but rather a description of the normal wear-and-tear process of aging. In the normal wear process of the spine, the soft central portion of the disc loses some of its water content and begins to dry out. This process usually begins at about the age of 20 years old and proceeds throughout one’s lifetime. Given this definition, a 25 year-old will show signs of degenerative disc disease when, in actuality, it is a normal part of aging and not "disease" at all. In rare situations this condition can lead to a "mechanical" type of low back pain in which strenuous activity in a person who is not physically fit will cause some back pain. Degenerative disc disease, if it does cause symptoms, is usually treated with appropriate exercise, body mechanics, and an anti-inflammatory medication. Although degenerative disc disease is very often a diagnosis associated with the “need” for a spinal fusion. However, surgical decision-making should proceed very cautiously.
Facet syndrome. The facet joints are located at the back of each vertebra and "attach" the vertebrae together. These are the joints that connect the vertebrae together and allow them to move while keeping the spine in proper alignment. In facet syndrome there is an inflammation of one or more facet joints. Inflammation of these joints can produce referred pain, which is pain that is felt some other place than where it is being caused. A facet syndrome is usually diagnosed based on your symptoms. Often, there is an area of tenderness between one and one and one-half inches to the side of the spine in the lower back. Pressure in this area will cause discomfort and sometimes pain down into the buttock or thigh area. The pain is usually made worse by certain activities such as bending forward or backward, twisting to one side or the other, or standing on one leg. This syndrome is an uncommon occurrence and is not serious. Although it can produce pain, this usually resolves within two to three weeks. The treatment is usually the same as that for a sprain-strain. In rare instances, when the condition becomes chronic, it may be treated by an injection of anti-inflammatory and anesthetic medication into the irritated joint. An appropriate exercise program should be part of any treatment for a facet syndrome.
Arachnoiditis. Arachnoiditis is inflammation or scarring of the connective tissue (the spinal arachnoid) around the spinal nerve roots. Arachnoid literally means "like a cobweb" and this is how the condition looks on imaging studies. The most common cause of arachnoiditis is surgery. The symptoms include pain, numbness, and tingling in the legs. Arachnoiditis can be difficult to treat. Treatments might include pain medicines, physical therapy, or a cortisone injection. A spinal cord stimulator, which is a surgically implanted unit that delivers a mild electrical pulse to the spinal nerves to block pain signals from reaching the brain, may be useful in severe cases. Arachnoiditis does not always preclude spinal surgery if there are other problems, although one should proceed very cautiously. Arachnoiditis itself cannot be treated by surgery and there is always the risk that any spinal surgery will make arachnoiditis worse.
Spondylolisthesis and spondylolysis. Spondylolisthesis literally means "slipping vertebrae" and refers to a condition in which one vertebrae "slips" over another. This can be caused by a fracture or crack in part of the vertebrae. This fracture is termed a spondylolysis. Although this condition occurs for many reasons, both in childhood and adulthood, we will focus on the most common scenario.
The fracture of the vertebrae usually results from trauma occurring over a period of time during the teenage years due to sporting activities that involve repeated episodes of hyperextension (bending over backwards). Spondylolisthesis is most often seen in gymnasts, ballet dancers, and football players. Typically, a single episode of hyperextension does not cause a problem, but repeated episodes result in the actual break. Initially, the crack is so fine that it will not be visible on a regular x-ray. If this condition is suspected, it is appropriate to have a bone scan which can detect very fine cracks in the vertebrae (we will discuss what a bone scan is later on). A common possible indicator of this condition is back pain in a young person for more than one or two weeks. If the problem is diagnosed when it occurs (usually between 13 and 16 years old) it can be treated effectively and completely. Treatment usually includes a brace and restriction of activities for about 4 months to allow the fracture to heal. In very severe cases of "slipping", a spinal fusion surgery may be necessary. If this is unrecognized when it occurs in childhood, it can cause back problems later in life.
The other common type of spondylolisthesis is termed "degenerative spondylolisthesis". This condition is caused by severe wear and tear changes in the facet joints or connecting joints of a lower back due to a variety of different reasons. The most common location for this condition to occur is between the fourth and the lumbar vertebrae, with the fourth vertebrae slipping forward (toward your stomach) over the fifth vertebrae. In diagnostic lingo all types of spondylolisthesis are graded, I to IV, with the "I" being the least amount of slippage and the IV being the most.
Scoliosis. Scoliosis is a term that is used to describe a curvature of the spine. There are several different varieties but it is an unusual cause of low back pain in people under forty years old unless it is very severe. The most important element relative to scoliosis is whether or not it is progressive (curving more and more). A small percentage of scoliosis in the lower back is progressive and needs to be treated appropriately. In the majority of cases however a finding of "scoliosis" is not meaningful and requires no specific treatment. One should be warned that:
This diagnosis is commonly given as a reason for low back pain with recommendations for extensive treatment to straighten out the spine when, in fact, the scoliosis has nothing to do with the pain.
Curves under 20 degrees, which represent the great majority of scoliosis seen clinically, need no treatment and are not known to be causes of pain.
Osteomyelitis. Osteomyelitis is an infection in the vertebrae or bones of the spine. It is very rare and includes symptoms of back pain while resting, loss of weight, and fever. It is detected on a number of tests one of which includes abnormal blood findings. It is treated with a brace and appropriate antibiotics for three to six weeks.
Discitis. Discitis is a rare condition and literally means “inflammation of the disc”. Although the exact causes are unknown, it is thought to be due to a bacterial or viral infection in the disc space. This causes inflammation and pain. It is more common in people under 20 years of age, persons with diabetes, or other individuals that have immune system problems. It is treated by antibiotics if bacteria are the cause and a brace if it has occurred in a child.
Transitional vertebrae. A transitional vertebrae is often seen on x-rays and is not associated with a greater frequency of low back pain. This condition is found at the base of the lumbar spine where it connects to the sacrum. There can either be one extra lumbar vertebra or one less lumbar vertebra.
Coccydynia. Coccydynia literally means “pain in the coccyx”. This is pain in the bone at the very lower base of the spine known as the coccyx. It most often occurs as a result of trauma, usually a direct fall on the buttocks. It can result in persistent pain and tenderness just above the rectal area. Treatment usually consists of avoiding sitting on hard surfaces. The use of a donut-shaped cushion can be helpful to control the symptoms. In more resistant cases, the use of anti-inflammatory medication or a local injection of anesthetic and cortisone may be useful. There is recent research suggesting that a special type of biofeedback to teach the person to relax local muscle spasms can also be helpful. Surgery to remove the coccyx may be considered as a last resort in severe and chronic cases; although the success in terms of pain relief is not assured.
Other spinal fractures. Spinal fractures are almost always seen in one of two circumstances:
First, in a younger person following a severe trauma such as a motor vehicle accident or a fall.
Second, in a person who has had a weakening of the bones of the spine due to a disease process such as osteoporosis or cancer of the spine.
In the latter situation, these patients are prone to experience a compression fracture of the vertebra due to this weakening. A typical warning sign of a possible spinal fracture would be a forty-year old person who develops back pain that:
· is not associated with activity · is so severe it can awaken him or her from sleep · does not resolve within a week or two
Such a person should be evaluated immediately by a physician who is familiar with spinal problems.
Subluxation. Subluxation is a term that is frequently used by chiropractors and osteopaths to explain the underlying reason for low back pain. The term is often used to indicate some type of limitation of movement in a joint. Various chiropractic treatments are used to restore the joint which is purported to be "subluxed" or restricted. This diagnosis is controversial among physicians who treat spinal problems and not all doctors are convinced that subluxed joints actually exist and are the cause of pain. Lumbar spinal stenosis. Lumbar stenosis means a narrowing of the spinal canal that causes a compression or "pinching" of the nerves passing through the area that go to the buttocks and legs. The stenosis can occur for many reasons including:
· disc bulges · severe wear and tear change leading to bony spurs · congenital (meaning from birth) narrowing of the spinal canal
Whatever the cause, the result is that the spinal canal through which the nerves pass is made smaller. Lumbar stenosis most typically presents itself as pain that:
Limits the person's ability to walk for any great distance or at a fast-paced
Is relieved if the person leans forward at the waist as the person walks.
Is relieved if the person sits down for a short period of time or until the symptoms subside
The reason that leaning forward decreases the symptoms is that this posture helps open the spinal canal space thereby temporarily decreasing pressure on the nerves. The diagnosis of lumbar stenosis is made from the history, physical examination, and imaging studies. This diagnosis becomes more and more common in the elderly population with each year over age 65 years old due to aging changes of the spine.
Although the condition usually worsens with time, it does not lead to paralysis, a shortening of life, or a loss of life. The most common consequences are limitations in activities and, in most cases, the progression of symptoms is slow. The treatment consists of three phases:
First, an appropriate exercise program combined with short-term use of anti-inflammatory medication
Second, a "low volume" epidural injection of medication into the space surrounding the spinal nerves which can give temporary relief
Third, a surgical widening of the spinal canal which includes a laminectomy (removal of the lamina) which gives the nerves more room
Chronic back pain syndrome. The chronic back pain syndrome is a group of symptoms that can occur as a result of back pain that goes on for more than about six months. The process by which this occurs has been termed physical and mental deconditioning by Dr. Robert Gatchel. The idea is essentially the same as the idea of, "if you don't use it, you'll lose it". The chronic back pain syndrome worsens over time and includes physical and psychological symptoms. It is important to note that:
Treatment for the chronic back pain syndrome almost always includes a multidisciplinary approach in which all aspects of the problem are treated simultaneously:
· Physical exercise and reactivation to address the deconditioning syndrome · Psychological intervention to address the mental deconditioning and emotional issues · Detoxification to address medication dependence and substance abuse problems · Return to work or other activity that provides a sense of purpose
For more detailed information on the evaluation and treatment of the chronic pain syndrome, refer to the Chronic Pain Management Series of courses.
The failed back surgery syndrome. Unfortunately, the failed back surgery syndrome is all too common. The symptoms are similar to the chronic back pain syndrome discussed previously, except that it follows some type of spine surgery. The failed back surgery syndrome can occur for a variety of reasons such as:
· early infection after spine surgery · a spinal fusion surgery done at the wrong level · psychological distress · inadequate re-conditioning after surgery · a spinal fusion surgery that does not heal properly (pseudoarthrosis) · some other physical problem (stenosis, arachnoiditis, etc)
In our opinion, the most common reason for the failed back surgery syndrome is that:
· The wrong patient was given the wrong surgery at the wrong time
Consistent with this view, we feel the best treatment for the failed back surgery syndrome is to avoid creating it in the first place, and that is the goal of pre-surgical screening. If the failed back surgery syndrome has already occurred, the treatment virtually never includes more surgery. It usually includes a conservative, nonsurgical approach similar to that used for the chronic back pain syndrome that focuses on physical and psychological issues simultaneously.
CONSERVATIVE TREATMENTS
It is beyond the scope and focus of this course to review all of the available conservative treatments for the various spine diagnoses discussed previously. However, if one becomes involved in presurgical screening, it is important to have some idea about what constitutes a reasonable course of conservative treatment. Many of the conservative treatments are reviewed in the chronic management pain series. Others, just to name a few, include chiropractic, physical therapy, and acupuncture. Conservative invasive pain management techniques include such things as epidural steroid injection, nerve block, facet blocks, and rhizotomies.
Reviewing available medical records is often a component of the presurgical screening. It is not uncommon to find in the surgeon’s assessment a statement like, “The patient has failed conservative treatment and desires to pursue the surgery option.” Upon questioning the patient during the clinical interview the practitioner may find out that the “failure” of conservative treatment amounted to 6-8 weeks of modality-oriented physical therapy (hot packs, ultrasound, and massage) and some medications. In many cases, this would not constitute an adequate trial of conservative treatment. This issue will be discussed further in the section that addresses what to do with patients who are not cleared for surgery. In these cases, very specific multidisciplinary treatments have been found successful.
DIFFERENT TYPES OF SPINE SURGERY
In the following section, we will review the most common types of spine surgery. In the vast majority of cases, patients referred for pre-surgical psychological screening will be facing one of the more extensive procedures such as a fusion or motion-preserving operation (e.g. artificial disc replacement). Even so, in order to be thorough, we will also review the less invasive procedures as well. Further detailed information on any of these procedures can be found at www.spine-health.com.
Why Do I Need to Know this Stuff?
It is important for anyone doing pre-spine surgery psychological screening to be at least somewhat familiar with all aspect of spine care including anatomy, diagnostic testing, and surgical procedure. This knowledge will help you direct your clinical interview appropriately, assess the patient’s understanding of the surgery that is being proposed (informed consent), and establish credibility with the patient. Very frequently, patients will have done some research regarding the proposed surgery and want to discuss aspects of it, at least in general terms. You can imagine how the clinical interview might proceed if the evaluator did not know the nomenclature for identifying vertebral levels (L3, L4, S1, etc), could not describe the difference between a microdiscectomy and anterior-posterior fusion, or could not discuss why the risk of paralysis from lumbar surgery is so low. Microsurgical Discectomy
This operation is minimally invasive and done with a microscope. It requires a laminotomy which is a partial removal of a small amount of the lamina which is the bone covering the spinal canal. (See an animated video discussing microsurgical discectomy procedures.) The patient is hospitalized the morning of the procedure, which is done under general anesthesia and can take anywhere from 45 minutes to several hours depending on what has to be done. The procedure generally requires only a very small incision from one to one and one-half inches. Microsurgical discectomy for a herniated disc is indicated for sciatic pain that does not respond to conservative treatment, progressive neurologic loss causing significant problems in daily functioning, spinal stenosis in older patients associated with a disc herniation causing the sciatica pain, and recurrent disc herniations. The pain following this type of surgical procedure is usually not severe and can be controlled with appropriate pain medicines. The local discomfort from the surgery usually goes away within several days. However, the sciatica can take quite some time to disappear depending on how long the nerve has been irritated prior to surgery, nerve re-growth factors, and other things. We like the tell patients to think of this continued nerve pain as "good pain" as it often indicates nerve regeneration. More detailed post-operative recovery guidelines are provided elsewhere by Dr. Goldstein.
Other procedures that might be done during a microdiscectomy are called a "laminotomy" and/or "foraminotomy". A laminotomy involves creating a small opening through the lamina allowing access to the spinal canal. A foraminotomy involves making a larger opening in the foramina to relieve nerve root compression. As discussed in the anatomy section, the “foramina” is a natural opening or "hole" in the spinal canal that allows the nerve root to exit and join with other nerves to form the sciatic nerve. These procedures are generally done to make room for neural structures that are being compressed.
The risks of microsurgical discectomy include infection, injury to the nerve root, problems with the anesthesia, a blood clot, and recurrent disc herniation. In order to prevent infection, an antibiotic is given intravenously at the time of surgery and occasionally eight hours following the surgery. Necessary manipulation of the nerve root during surgery can result in injury causing numbness and/or weakness in the area of the nerve distribution and this will resolve in most cases. There is an approximate 4 percent chance of a recurrent herniation of additional disc material at the operated level. This is due to the fact that no attempt is made at the time of surgery to remove the entire disc, rather only that portion that is causing irritation or compression of the nerve root. If reherniation occurs, there will usually be a pain-free interval after the successful microsurgical discectomy and then a sudden recurrence of sciatic pain. This recurrence is almost always due to a recurrent disc fragment, and often the pain is much more intense than the original sciatica. In about 30 to 40 percent of these reherniation cases, oral steroids and or one or two epidural blocks will sometimes successfully treat the problem. In about 60 to 70 percent of the reherniation cases, repeat surgery is required and is usually quite successful. Laminectomy
A laminectomy is the surgical removal of the lamina and associated ligament in order to access a herniated disc which is then removed. Removing the herniated disc alleviates the pressure and/or irritation on the affected nerve roots. A laminectomy might also be done to take the pressure off the spinal canal in cases of spinal stenosis. A laminectomy can also be an appropriate treatment for those individuals who have had prior surgery with recurrent and/or residual problems requiring additional removal of bone in order to make more room for the nerves. The hospital stay is typically to 2 to 5 days; although, in an elderly person, additional hospitalization in an extended care facility may be required for up to several weeks. This allows for additional rehabilitation and recovery time in this population.
Because a laminectomy is done primarily in conditions of spinal stenosis, the recovery and resolution of symptoms is longer than it would be following surgery for sciatica due to a simple disc herniation. We advise our patients that recovery can take four to six months or sometimes even longer. Postoperative rehabilitation often requires physical therapy starting approximately two to three weeks after the operation. The risks associated with a laminectomy are similar to that for a microsurgical discectomy. The risk of infection or blood clot is somewhat greater than in the microsurgical procedures due to the longer operating time. The risk of disc herniation and need for re-operation after a laminectomy is between four and six percent. Spinal Fusion
The primary indication for a spinal fusion is for the alleviation of "mechanical" low back pain. This is pain that is made worse by activities such as bending, twisting, and lifting. A fusion is usually recommended if some type of instability is seen between two vertebrae. This is usually assessed by looking at "bending" x-ray films in which the patient bends forward and backward while x-rays are taken and evaluated in both positions. Except in rare cases, spinal fusions are not indicated for leg pain. The purpose of any type of fusion is to stop the motion that naturally occurs between two vertebrae (the functional unit). Spinal fusions are generally used to treat degenerative disc disease and spondylolisthesis (one vertebra slipping over another). There are now many different types of fusions and it is beyond the scope and purpose of this course to review all of them. The pre-screening psychological screening issues remain the same regardless of the type of fusion (or motion-preserving surgery to be discussed subsequently) the patient is undergoing. The most common types of fusions are as follows:
Posterolateral gutter fusion. This procedure is considered the gold standard of the spinal fusion procedures and has been around for decades. The majority of fusions are done using a posterior approach (“from the back”). In these procedures, the lamina is removed (the portion of the vertebra that covers the spinal canal). Any bone that may be pinching a nerve root is removed. Fresh bone (bone grafts), either taken from the patient's iliac crest (autograft) or a cadaver bone from a bone bank (allograft) is then placed at the sides (posterolateral) of the vertebrae to be fused with the goal that eventually the two vertebrae will grow together. After the bone graft is placed, instrumentation is used including pedicle screws (that go into the pedicles of the vertebrae) and rods that are secured between the heads of the screws. Using these screws and rods has been shown to enhance fusion rates and help with getting the patient more active sooner after the surgery. As the vertebrae grow together they form one solid unit with almost no motion between them. (See a spinal fusion animated video).
Posterior lumbar interbody fusion (PLIF). This procedure is similar to one discussed previously but the damaged disc is partially removed and some of the disc wall is left behind to contain the bone graft material. In the PLIF the bone graft occurs in the empty disc space. A video of the procedure is available for review at PLIF.
In reviewing records or interviewing patients as part of a pre-surgical screening, you may also hear about bone morphogenetic proteins (BMP) being used. BMP stimulate bone growth that naturally occurs in the body. These proteins that exist in the body can be produced, concentrated and placed in the area of the spinal fusion and can create a fusion without the need for any use of the patient’s own bone. Since BMP is quite expensive, one generally sees it recommended in cases where there is an increased risk of non-fusion (pseudoarthrosis) such as smokers or a case of a previous failed fusion.
Anterior lumbar interbody fusion (ALIF). This type of fusion is done from the front of the spine. There are different methods to allow surgical access to the anterior spine:
A more open procedure requiring an incision of about 3 to 5 inches in the abdomen area and retraction of abdominal muscles (rectus abdominis) and abdominal contents (in the peritoneum).
A minilaparotomy method uses one small incision, allows for good visualization and helps diminish postoperative pain
An endoscopic approach that utilizes several one-inch incisions but results in less visualization and requires greater surgical times. This method is falling into disfavor.
An ALIF is usually done with the assistance of a vascular surgeon since mobilization of large blood vessels is required. After the large vessels are moved to the side, the spine surgeon proceeds with removal of the disc material and the grafting procedure (bone and bone/interbody cages) is completed.
The ALIF is often combined with posterior approach (anterior-posterior fusion) to provide more rigid fixation than an anterior fusion alone. Anterior-posterior fusions might be necessary for people who have had failed prior surgeries, who are smokers, or who have had prior complications such as infection. In these cases (that need to be carefully selected) two separate surgical procedures are done, either under a single anesthetic or several days apart.
Lateral lumbar interbody fusion (XLIF), Transforaminal Lumbar Interbody Fusion (TLIF). These techniques will not be discussed in detail and information is available elsewhere (see previous links for more detailed articles). These procedures are similar to the PLIF but the surgical approach is different and designed to minimize tissue damage. For instance, the XLIF uses two small incisions in the patient’s side designed to avoid major muscles and nerves. As such, the recovery time is less. (See XLIF video and TLIF video for additional information).
Risks and complications. The risks associated with a spinal fusion are significantly greater than those associated with the other surgeries we have discussed previously. Even so, the relative risks are still low. Risks more specific to spinal fusions include a failure or breakage of the instrumentation, pain in the hip where the bone graft is taken from, infection, and failure of the vertebrae to fuse or grow together (pseudoarthrosis). Another risk that should be noted is in people who smoke. Smokers have been shown in studies to have significantly less of a chance of obtaining a successful fusion (as low as 60 percent compared with 85 percent or more in the nonsmoking population). Consideration of the risk and benefit ratio should be done with great care when considering a spine fusion surgery given the greater length of time off of work, the significant cost, and the longer rehabilitation time associated with this major surgery. There are additional risks associated with an anterior fusion including damage to the large blood vessel resulting in excessive blood loss (1 to 15% occurrence rate) and, in males, creating a condition known as retrograde ejaculation (ejaculation into the bladder) due to nerve damage from the surgery (occurrence rate of less than 1% and tends to resolve over time postoperatively).
Motion Preserving Surgeries
Traditionally, spinal fusion surgery has been the treatment of choice for mechanical low back pain. One problem with fusing one or more vertebral levels is that it places greater forces on levels above and below the fusion. It is thought that, over time, this can result in degeneration at these levels due to the increased stress. The idea of preserving motion was developed in response to these issues and borrowing from successful experience with other joint replacement technology (e.g. hip, knee, shoulder).
Artificial disc replacement (ADR). ADR has been done in Europe for many years and is now approved for use in the United States beginning in about 2004. Aside from preserving motion, another goal of ADR is to relieve pain by replacing a diseased or damaged disc. In the procedure a small incision is made in the abdomen and the diseased disc is removed. The end surfaces of the vertebral bodies are cleaned of all diseased disc cartilage and prepared for insertion of the metal endplates. The vertebrae are then separated to relieve pressure on the nerves and allow for insertion of the prosthesis. Metal implants are anchored to each vertebral endplate and the polyethylene sliding core is then inserted in between. The spine is then returned to its normal posture which seats the endplates and prosthesis (See ADR for an animated video).
This technology can be very seductive to patients since it is the “latest thing” and conceptually makes common sense (e.g. preserve motion). Part of pre-surgical screening includes helping patients make informed decisions. This is done by directing them to reliable health information. The California Technology Assessment Forum has recently updated its review of ADR versus fusion (2009).
Posterior Dynamic Stabilization Systems (PDSS). Although there are many devices in development, one motion preserving alternative to ADR is PDSS. These devices are best described as an internal brace that allows controlled movement of the problem segment of the spine. Most of these devices are derived from pedicle screw and rod constructs that were developed for spinal fusion surgery as discussed previously. For a spinal fusion, those devices are designed to provide rigid stability to ensure a fusion (complete stabilization and no motion). Rather than having rigid screws and stiff metallic rods, this group of devices has such components as screws and cords or flexible rods. The goal of the new generation of devices is to allow controlled motion in such a way as to achieve more normal movement of the spine. Several of these devices have been developed and are in various stages of testing and approval. Most of them have only been used outside of the United States. These devices are typically used to treat patients with symptomatic spondylolisthesis or degenerative disc disease. Some devices are also being studied for the treatment of lumbar spinal stenosis. PRE-SURGICAL SCREENING
The process of the pre-surgical screening will include (1) assessing predictor variables for spine surgery success or failure, (2) getting some idea of the patient’s understanding of what type of surgery is being recommended along with his or her comprehension of the risks and benefits (informed consent), and (3) having an open discussion with the patient about the surgery decision. In going through this process, you may or may not have the assistance and cooperation of the surgeon. Although some surgeons do rely on pre-surgical screenings as part of their practice, these are also commonly done as referred by the insurance company or some other party to help determine if the patient has a reasonable chance of benefitting from the elective procedure. Often the referral question also includes whether there are other less aggressive treatments that might be more appropriate.
The Purpose of Screening and What Constitutes a Successful Surgery?
The purpose of a presurgical screening addresses three important questions:
Is the patient competent to make an informed decision about spine surgery? Answering this question involves an assessment of the patient’s capacity to make an informed decision about having a spine surgery. Being sure there is informed consent is ultimately the responsibility of the surgeon; however, the pre-surgical screening can highlight any problems that might occur relative to making sure the patient understands the nature of the proposed treatment, the risks and likelihood of success, and available alternative treatments. Additional information about informed consent can be found in another course (Ethical Issues).
Is the patient at significant risk for psychiatric decompensation as a result of proceeding with an elective spine surgery? Although it is not common to evaluate a patient who presents with a risk of psychiatric decompensation after spine surgery, it does occur. In these cases, the usual scenario is a significant risk for a worsening of the depression and chronic pain syndrome if the patient’s results do not match his or her pre-operative expectations. If a significant risk is identified, specific treatment may be recommended prior to the surgery.
Are there significant biopsychosocial factors that would preclude a successful clinical response to the surgery? This question is really the primary focus of the course. This involves assessing specific predictor variables and determining if there is a significant risk of clinical failure in response to the proposed surgery. It is important to keep in mind two caveats when doing pre-surgical screenings: (1) you are not assessing whether the patient can psychologically manage or emotionally survive the surgery process. You are actually making a determination relative to the likelihood of success. (2) given current technology and the skill level of most spine surgeons, most spine surgeries are technically successful. The presurgical screening is directed at assessing likelihood of clinical success. Clinical success might be defined as decrease pain ratings, improved function, decrease need for medication, change in disability status (e.g. return to work), improved social function and relationship, and improved quality of life.
The following will discuss the predictor variables commonly included in a pre-surgical screening. Since hundreds of predictor variables have been researched, we are only including those that have consistently been shown to have some predictive power. It must be underscored that no one variable provides for adequate screening; rather, one must evaluate a pattern of results for multiple variables. BIOLOGIC-LIFESTYLE VARIABLES
Although a number of biologic, demographic and lifestyle variables have been investigated (See Table 2), most have shown inconsistent predictive power when assessed independently. Of these variables, cigarette use, alcohol and substance use, obesity, exercise are the most useful to include in a screening.
Cigarette Use. An extensive amount of research has firmly established that cigarette smoking is detrimental in patients undergoing lumbar fusion surgery. Smoking is related to a number of problems in patients undergoing spinal fusion including the following: (1) a decreased rate of successful fusion called non-union or “pseudoarthrosis”, (2) a decreased rate of clinical outcome regardless of successful fusion, (3) a limitation in functional rehabilitation post-operatively, and (4) poorer overall patient satisfaction with the spine surgery.
Studies have demonstrated that the rate of non-fusion in smokers is as much as twice that found in non-smokers. Although the studies on non-fusion rates are highly variable depending upon the procedures used, the rates for non-smokers is about 5% to 15% whereas in smokers it is approximately 20% to 30%, or higher. Most theories as to why this occurs relate to the negative effects nicotine has on bone growth (which is essential for a successful fusion). One of the most deleterious effects of nicotine is decreased revascularization of the bone graft. In essence, the bone graft does not get enough nutrients due to a lack of blood supply and, therefore, does not grow. Another recently discovered effect of nicotine is that it may have anti-inflammatory effects, which also interfere with fusion healing.
Not only does smoking affect the actual fusion, but it has also been found to be associated with other outcomes to spinal fusion surgery. These negative effects of smoking have been found in patients regardless of whether or not the fusion was actually successful. When smokers and non-smokers with successful fusions are compared on many other outcomes measures, the non-smokers typically do better overall. This is probably due to the fact smoking affects spine and other health issues. For instance, smoking has been found to accelerate the rate of disc degeneration and this might contribute to ongoing spine problems even after a spinal fusion. Also, smoking is related to a number of other health issues (e.g. cardiovascular and pulmonary disorders, etc.) that might interfere with a spinal fusion patient regaining a return to normal function. In addition, cigarette use has been correlated with “unhealthy” lifestyle behaviors (e.g. lack of exercise, poor nutrition, alcohol use, etc.), lower SES, heavy physical job demands, and these impact spine surgery outcomes independent of the fusion issue.
An excellent study by Glassman et al. (2000) investigated the effects of smoking and smoking cessation on spinal fusion outcomes. As part of their analysis, they looked at the return to work rate in smokers versus non-smokers, all of whom had a successful spinal fusion surgery (they had a solid fusion). The investigators found the following return to work rates:
· 51% for patients who never quit smoking before or after surgery · 68% for patients who quit smoking for longer than one month after surgery · 77% for patients who quit smoking for longer than 6 months after surgery · 71% for patients who were non-smokers
As can be seen, even in patients with a successful fusion, smoking had a negative impact on return to work. Interestingly, for those patients who were able to quit smoking for an extended period of time, their return to work rate was similar to the non-smoking group. The Glassman et al. (2000) study also found that non-smokers were more satisfied with the surgery outcome overall, even when comparisons were made only for patients who obtained a solid fusion. Amount of smoking also had an effect on satisfaction. Smoking groups of less than a pack per day (PPD), one to two PPD, and greater than two PPD were compared. It was also found that the more a person smoked, the more dissatisfied he or she would be with the spinal fusion surgery overall. The results of the Glassman (2000) study are consistent with previous research done in this area.
In many cases, the surgeon will go ahead with the surgery, even in a patent who smokes, while using alternative surgical procedures to help offset the negative influence of smoking. Some of the most common methods to help offset the negative effects of smoking are rigid stabilization approaches. This might include such things as pedicle screw fixation and anterior-posterior fusion (circumferential fusion). Other procedures might also be used including interbody grafting techniques, bone stimulators and/or use of BMP. Even with all of these additional efforts to achieve a solid fusion in a patient who smokes, the non-union rate is still a significant problem. Even so, smoking cessation is supported as the most ideal way to address this issue.
Based upon the previous discussion, the best approach for smokers facing spinal fusion (or other spine surgery) is to stop smoking and stay abstinent. This results in the best outcomes including a solid fusion and other outcomes. However, research consistently demonstrates that this is easier said than done. The Glassman et al. (2000) study nicely exemplifies this problem. All patients in the study were recommended to stop smoking before the surgery and to continue to abstinent post-operatively. Of the 188 patients who smoked, 125 were able to quit for at least some length of time and 63 did not quit at all. Typically, patients who do not quit prior to surgery make a commitment to stop immediately after the surgery, although this was not specified in the article. Of the 125 patients who quit, 74 stopped for less than 1-month prior to surgery and 51 stopped for greater than 1-month prior to surgery. Table 12 represents how each group of smokers did with their smoking cessation post-operatively based upon the length of time they were able to quit prior to surgery:
As can be seen, successfully quitting smoking after the surgery is highly unlikely if the patient has not done so pre-operatively. This is consistent with what we see in the spine surgery practice. We have many patients who tell us with great conviction that they will smoke until the spine surgery and then quit afterwards. In the overwhelming majority of cases, the patient is not able to quit smoking post-operatively, or only does so for a brief period of time. The recovery from a spine fusion surgery is stressful physically, mentally and emotionally. Patients will often tell us that the first two months of recovering are especially tough due to acute pain from surgery healing, functional restrictions, and just “boredom”. It is exactly these factors that induce a smoker to use cigarettes to “pass the time”, enjoy a rewarding experience, “deal with the stress”, etc. Another interesting finding in the study is the longer a person has been abstinent from smoking prior to the surgery, the greater likelihood he or she will be able to maintain being a non-smoker post-operatively. This information might provide some guidelines for patients and surgeons relative to preparing for spine surgery, including smoking cessation.
The Glassman study was also able to investigate how the amount a person smokes affects ability to not smoke after spinal fusion. Of the 125 patients who were able to stop smoking for any length of time before surgery, the amount the person smoked prior to surgery predicted their ability to stay abstinent. This can be seen in Table 13.
The results are consistent with common sense: the more you smoke the harder it is to quit and stay abstinent. This is true even if patients know that returning to smoking threatens the outcome of their surgery. The data also show that it is difficult to give up smoking over the long term (6 months or greater) for all levels of cigarette use. More detailed information regarding smoking and spine surgery is available including information on quitting smoking interventions. Alcohol and substance abuse. It is difficult to accurately assess alcohol or substance abuse in spine surgery candidates since many patients are reluctant to reveal this type of information. As a result, very few studies have directly examined the effect of alcohol and/or substance abuse on spine surgery outcome. Excessive alcohol use has the potential to negatively impact a patient’s recovery from spine surgery in a number of ways including slower wound healing, sleep disruption, increased depression and anxiety, increased likelihood of smoking due to lowered impulse control, poor nutrition, amplified endocrine changes in response to surgery and synergistic interactions with medications (See the course Surgery Preparation I: Conceptual Models for a discussion of the psychoneuroimmunology of surgery).
Substance abuse in spine surgery candidates might include use of illicit drugs (current or history) or abuse of prescription medications. With the increased acceptance of long-term opioid treatment in the management of chronic pain conditions, evaluation of the possible abuse of prescription medications becomes more difficult. As part of the screening, the practitioner should assess the following questions: what is the overall level of pain medication use, is the patient showing a need for escalating dosages, has the medication actually improved patient function, is the patient taking the medications as prescribed (compliance or noncompliance), is there any evidence of abuse of prescription medications (e.g. doctor shopping, frequent emergency room visits, getting medication from illegitimate sources), are all the patient’s medications related to the chronic pain problem being managed by one physician, and is the patient under an opioid treatment contract. If there is any evidence of alcohol or substance abuse, or if the patient has been on high doses of opioids for quite some time, it is most prudent to address these issues prior to surgery. In assessing pain medication use, it is important to be aware of key concepts including tolerance, pseudotolerance, physical dependence, addiction, and pseudoaddiction. An overview can be seen in Table 14 and a more detailed discussion can be found in the Chronic Pain Management III: Special Issues or QME Chronic Pain Management III: Special Issues courses.
Obesity. Although it seems that body weight would be a reasonable predictor of diminished spine surgery results, this has not been consistently found in the research (See Block et al., 2003; Mannion and Eflering, 2005; Deardorff, 2010 for reviews). However, obesity has been found to contribute significantly to a number of other variables that are predictive of poor outcome to spine surgery. For instance, Gepstein et al. (2004) found that the percentage of very dissatisfied patients after spine surgery was significantly higher among obese patients and that increased body mass index had a negative effect on pain perception, and activities of daily living after surgery.
Patel et al. (2007) studied 97 obese patients (BMI greater than 25; mean BMI=28.8) that underwent elective thoracic and lumbar spine fusion surgery (anterior, posterior, or anterior-posterior). Of these, there were 42 complications in 31 patients (37%). It was found that the chance of significant complication was associated with increasing BMI (BMI of 25:14%; BMI of 30: 20%; BMI of 40: 36%). Complications included such things as wound infection, cerebrospinal fluid leakage, deep vein thrombosis, cardiac events, pneumonia, and prolonged intubation. The authors discussed that their study documented a correlation between obesity and perioperative complications. In a similarly designed study, Vaidya et al. (2009) found that postoperative complications were significant in 45% of morbidly obese patients and 44% of obese patients. The authors conclude that obese and morbidly obese patients have multiple comorbidities resulting in perioperative complications.
LaCaille et al. (2007) investigated the effects of obesity and litigation on costs in a workers’ compensation patient population that underwent interbody cage lumbar fusion (ICLF). The authors concluded that, “The present investigation also found that patients considered obese (body mass index >30) had 61% (nearly $18,000) greater compensation expenditures than did their nonobese counterparts undergoing ICLF” (p. 270). These results suggest that including obesity as one of many important predictive variables to be assessed is appropriate.
Exercise and activity level. Surprisingly, very few studies have investigated the predictive power of pre-operative level of exercise to surgical outcome (See Block et al., 2003 for a review). In one study, Dolan et al. (2000) compared the effects of a post-operative exercise program to a control group. Those patients undergoing the post-operative exercise program demonstrated better results relative to reduced pain levels and disability as well as improved muscle endurance and mobility. In other studies, better pre-operative walking capacity predicted better post-operative walking capacity along with improved satisfaction (See Aalto et al., 2006 for a review). Although exercise may not have been investigated directly relative to predicting spine surgery outcome, it certainly relates to the physical deconditioning aspects of the chronic pain syndrome (See chronic pain management series for a complete discussion of the chronic pain syndrome: Chronic Pain Management III: Special Issues or QME Chronic Pain Management III: Special Issues. In addition, those patients who do engage in regular exercise, regardless of their back pain, might be expected to show higher levels of self-efficacy, less fear of pain, and a better health outlook overall. As will be seen in the evaluation report examples, we use the Multidimensional Pain Inventory (MPI) to obtain a general assessment of activity and identify a physical deconditioning syndrome (the MPI is discussed in greater detail subsequently under spousal relationship issues). WORK-RELATED VARIABLES
Work-related variables, as a group, demonstrate some of the strongest correlations with poor spine surgery outcome. Those variables amenable to presurgical screening include being in the workers’ compensation system, litigation, and extended disability duration.
Workers compensation. A great number of studies have demonstrated that involvement in the workers’ compensation system predicts a poorer outcome to spinal surgery (See Block et al., 2003 for a review). Although it might be concluded that this is related to financial incentives for staying disabled, it is more likely due to the various difficulties experienced by the disabled worker including such things as financial distress, loss of identity related to the job, an adversarial relationship with the employer and insurance carrier, delays in treatment, having to “prove” one is injured, among other things. The longer the patient is off of work, the more time a “system-induced functional disability syndrome” has to develop. Although workers’ compensation status is a significant predictor of spine surgery outcome, studies suggest that this effect is mediated by other variables such as time off of work, legal representation, job satisfaction, etc. (Gatchel and Turk, 1999; Hagg et al, 2003; Mannion and Elfering, 2005). In an interesting study relative to this issue, Anderson et al. (2006) investigate work status as a predictor of surgical outcome of discogenic back pain. In the study, 106 patients underwent ALIF after imaging, discographic and presurgical psychological screening evaluations. All patients had chronic pain greater than 6 months. Of the 56 patients disabled from work before surgery, 24 returned to work, while 45 of 49 workers remained working. As such, the preoperative work status was a statistically important predictor of surgical outcome. The authors conclude that, “Patients working at the time of surgery were 10 times more likely to be working at follow-up.”
For the patient who loves his job and is undergoing a spine surgery for a disc herniation that occurred at work just two months prior, workers’ compensation status will rarely be a predictor of poor outcome. However, for the patient who was injured at work and has been disabled for over 1-year (along with other predictor variables), being in the workers’ compensation system becomes a significant predictive variable.
Litigation. Another predictor variable that has consistently been linked to poorer spine surgery outcome is litigation status related to workers’ compensation, personal injury or disability benefits (See Deardorff, 2010 for a review). Although one might surmise that this is due to symptom exaggeration for secondary gain, it must be assumed that the spine surgery is being recommended because some evidence of pathophysiology has been identified (LaCaille et al., 2005). The litigious patient might very well do poorly because of increased somatic sensitivity to pain as a consequence of financial incentives and social-contextual variables.
Duration of Sick Leave. Lengthy pre-operative sick leave is a consistent predictor of diminished response to spine surgery including global outcome, overall satisfaction, back-specific function, and return to work. Longer duration of sick leave allows for development of the functional disability or chronic pain syndrome which is probably the reason for the poorer spine surgery outcomes. The chronic pain syndrome is explained in more detail in other courses: Chronic Pain Management I: Concepts or QME Chronic Pain Management I: Concepts.
Job dissatisfaction. Job dissatisfaction has been found to be predictive of work injury and delayed recovery. Although there is not much research directly assessing its impact on spine surgery outcome, it may be useful to assess as part of pre-surgical screening. From a common sense and behavior standpoint, if a patient with a successful spine surgery outcome is “rewarded” by having to return to a job that he or she despises, the chances that the patient will acknowledge improvement will be diminished. The Block et al. (2001) study found that job dissatisfaction as assessed during the interview was predictive of surgery outcome. Whether or not job dissatisfaction should be assessed will depend on the circumstances. If the case is an injured worker and the employer is holding the job position until the treatment is complete, then job satisfaction should be assessed. If there are no vocational issues relevant to the spine surgery outcome, then assessing job issues may not be necessary (e.g. the patient will not return to the previous employment, the patient is retired, the patient is medically disabled, etc.). Job dissatisfaction may be assessed during the clinical interview, through the use of objective measures (e.g. the Job Dissatisfaction Scale of the BHI-2).
PSYCHOLOGICAL FACTORS
Psychological factors are among the most frequently investigated predictive variables for spine surgery outcome. Some of the common psychological variables assessed include pain sensitivity, depression, anxiety, anger, fear avoidance, severe psychopathology, and various personality disorders or features. Psychological predictive variables are often assessed through the use of psychometric testing. Pain Sensitivity
Of all the psychological factors investigated, those falling under the rubric of “pain sensitivity” have shown the most consistent predictive power. Pain sensitivity might be defined as a patient’s propensity to display pain behaviors beyond what would be expected due to nociceptive input and objective findings. Pain sensitivity also encompasses the idea of how much the patient is “suffering” due to the pain; or, the emotional contribution to the patient’s perception of pain and level of disability. Pain sensitivity includes such concepts as heightened somatic awareness, fear of movement (kinesophobia), somatic anxiety, and general psychological distress (but not, necessarily, depression). Given this conceptualization of pain sensitivity, it is not surprising that any test that assesses some component of this construct might predict poor spine surgery outcome. This is probably why many tests (aside from the MMPI-2) have been shown to correlate with spine surgery outcome including the Distress Risk and Assessment Method (DRAM; Trief et al., 2000; Main et al., 1992), the Dallas Pain Questionnaire (Anderson et al., 2006), the Mental Component Score of the SF-36 (Trief et al., 2006), Waddell Non-Organic Signs (Spratt et al., 2004), among others. We will provide an overview of commonly used measures of pain sensitivity. Certainly, others are available and might be utilized depending upon practitioner preference. We recommend using more than one measure so that results can be analyzed in terms of convergent validity. MMPI-2. For a complete overview of the MMPI-2 and its use with chronic pain patients, see the Chronic Pain Management II: Evaluation and Treatment or QME Chronic Pain Management II: Evaluation and Treatment courses. The original MMPI was the most commonly used standardized personality test with chronic pain patients. The original MMPI was revised and released as the MMPI-2. Similar to its predecessor, it is likely that the MMPI-2 will also be the most commonly used personality test with chronic pain patients. It is beyond the scope of this course to discuss all of the issues related to using the MMPI-2 with chronic pain patients and the reader is referred elsewhere (See Deardorff 2000 for a review). The MMPI/MMPI-2 is the most widely researched and utilized test for presurgical screening. Block et al. (2003) summarizes a number of studies and some of the more interesting results are as follows:
In one study (Spengler et al., 1990), elevations on Hy and Hs contributed 26% to a multiple regression equation against predicting surgery outcome whereas imaging studies contributed only 10% and neurological signs only 3%.
In a predictive regression equation developed by Block et al. (2001), Hy was the strongest predictor of spine surgery clinical outcome exceeding medical variables of length of injury, type of surgery performed, and number of previous spine surgeries.
As discussed by Block et al. (2003), and supported by the above findings, the most important scales of the MMPI when assessing pain sensitivity are Scales 1 (Hs: Hypochondriasis) and 3 (Hy: Hysteria). As discussed by Block et al. (2003), both of these scales were designed to assess “an inconsistent relationship between organic pathology and physical symptoms” (p. 82). This is exactly the relationship that one would conclude is predictive of spine surgery outcome (consistent relationship = symptoms more likely related to organicity; inconsistent relationship = symptoms less likely related to organicity). After an extensive review of the literature, Block et al. (2003) conclude, “Thus, it appears that pain sensitivity, as assessed by the MMPI Hs and Hy Scales may predispose patients toward negative spine surgery results; even when surgery corrects the underlying pathology, patients with such characteristics may be unable to perceive any physical improvement” (p. 84). In our terminology, this situation represents a “technical success but clinical failure”. Consistent with recommendations by Block et al. (2003), when using the MMPI-2 for PSS, a T score of greater that 70 (rather than 65) is considered significant.
Battery for Health Improvement-2. The Battery for Health Improvement-2 (BHI-2) is a 217-item, self-report, multiple-choice instrument designed for the psychological assessment of medical patients. The purpose of the test is to provide relevant information and treatment recommendations to professionals who treat injured patients in a variety of settings, including physical rehabilitation, vocational rehabilitation, and general medicine. The BHI-2 has 18 scales organized into five domains: Validity scales, Physical Symptoms scales, Affective scales, Character scales, and Psychosocial scales. The BHI-2 was designed for patients 18-65 years old who are being evaluated or treated for an injury. The test was designed for patients with at least a 6th grade education and takes approximately 35 to 40 minutes to complete (See BHI Psychological Test Home Page for a review).
Unlike many psychological tests that have been adapted for use with medical patients, the BHI-2 was designed specifically for this clinical population. As discussed in The Manual (Disorbio and Bruns, 2003), self-report psychological tests tend to “overpathologize” what might actually be normal or expected for the average medical or rehabilitation patient. Thus, traditional psychological tests must be used with caution and interpreted accordingly by a qualified individual.
As documented in The Manual, research relative to the development of the test has been extensive. This has included establishing normative values, demonstrating reasonable reliability (internal, test-retest), and assessing validity by correlating BHI-2 scales with scales from other established instruments (e.g., MMPI-2, MCMI-III, etc.). The BHI-2 has not been directly tested in terms of its ability to predict spine surgery outcome. The use of the BHI-2 would be justified based upon its correlation with MMPI-2 scales that been shown to have predictive power. For instance, relative to pain sensitivity, the practitioner might be particularly interested in the Somatic Complaints Scale, Pain Complaints Scale, and Functional Complaints. The Somatic Complaints Scale is conceptualized as a measure of somatized physical symptoms associated with underlying depression and anxiety; as such, and it correlates with the MMPI-2 Hy-Obvious (Hy-O) subscale, Depression (D), and Anxiety (ANX, A) scales. The Pain Complaints Scale is a measure of diffuse, severe pain that is unlikely to be caused by any single injury or condition. It correlates with the Scored Pain Drawing, and the MMPI-2 HY-O and Hs scales. The Functional Complaints Scale is designed to measure the patient’s perception of impairment. It has been found to correlate with MMPI-2 scales of HyO, Hs, and D.
Pain Drawing. The pain drawing is another purported assessment of pain sensitivity and has been found to correlate with MMPI-2 Hs and Hy Scales (See Block et al, 2003; Carnes et al., 2006; Mannion and Elfering, 2005 for reviews). Pain drawings are hypothesized to identify the psychological contribution to a patient’s pain and are scored in a number of ways (Carnes et al., 2006). Pain drawings that are deemed “abnormal” or “non-organic” (unexplainable pain distribution) are thought to identify patients with a greater psychological component to their pain, although this conclusion has been contested
Pain drawing #1. The first pain drawing is considered abnormal since the symptoms do not follow anatomic distribution and the pattern is vague and diffuse. This drawing would meet two of the penalty point domains: poor anatomic localization and pain expansion. In this patient, after extensive objective testing, there were no factors identified that would
Pain drawing #2. The second pain drawing was considered abnormal since it met three of the penalty point domains: poor anatomic localization, pain expansion, and adding features or explanatory notes. The drawing also shows pain outside the body. Again, there were no objective findings that would explain these pain and symptom distributions.
Pain drawing #3. This pain drawing is probably the most fascinating I have come across in practice. This was a 23 year old male who was referred for a pre-surgical screening prior to a proposed spinal fusion. The pre-surgical screening was completed and the patient was not cleared due to biopsychosocial factors. It was also clear during the clinical interview that the patient was showing insidious onset of psychotic features (delusions, paranoia, disorganized speech, etc.) that would wax and wane. The patient had no history of psychiatric treatment or reported symptoms and his surgeons had simply
The DRAM System. The Distress and Risk Assessment Method (DRAM) was developed as a rapid measure of distress in back pain patients and to help evaluate the risk of poor treatment outcome (Main, et al., 1992). The DRAM is actually comprised of two brief instruments: a modified version of the Zung Depression Index (ZDI) and the Modified Somatic Perceptions Questionnaire (MSPQ). The ZDI is a self-rated measure of depression that was developed in 1965 and has been used extensively since that time (Zung, 1965). The MSPQ was originally developed by Main (1983) and is described as a test of heightened autonomic or somatic awareness (also termed “somatic anxiety”; Main et al., 1992). The MSPQ underwent extensive test development (Main, 1983). The modified ZDI contains 23 items that are rated by the patient on a 4-point scale (none-rarely to most-of- the-time). For use in the DRAM system, the modified ZDI items are scored from 0-3 with some items reversed scored (See Main and Waddell, 1984; Main et al., 1992). The range of scores on the modified Zung is 0 to 69.
The MSPQ contains 22 somatic items that are also rated on a 4-point scale (0-3; “not at all” to “extremely-could not have been worse”). Of the 22 items on the MSPQ, only 13 are used in obtaining an actual score. The range of scores on the MSPQ is 0-39. The total number of items on the DRAM is 45 and requires about 10 minutes to complete. The DRAM went through extensive test development as described in Main et al. (1992) and cluster analysis revealed four patient types: Normal (N), At Risk (AR), Distressed-Depressive (DD), and Distressed-Somatic (DS).
Type N patients are characterized by no evidence of distress and no abnormal illness behavior (low scores on all scales).
Type AR patients show slightly higher scores than N patients, with the largest differences in depressive symptomatology.
Type DD patients show clear elevations on all scales but most marked on depression.
Type DS patients also showed more elevations than Type N patients on all variables and show comparable levels of illness of behavior to DD patients but particular elevation on somatic awareness.
Main et al. (1992) then developed classification decision rules as follows:
The individual psychometric properties of the modified Zung and the MSPQ have been found to be acceptable and will not be reviewed here. The DRAM classification system has been validated for a number of uses. As discussed by Main et al (1992), “The DRAM is designed as no more than a first-stage screening procedure, whether as confirmation of clinical impression, or to alert the clinician that a more comprehensive psychological or psychophysiologic assessment is indicated (p. 50). The validity of the patient types was specifically investigated in Main et al (1992). The classification groups or patient types (N, AR, DD, and DS) demonstrated expected concurrent validity with other measures across categories of clinical features, pain and depression, cognitive factors, and personality structure. The DRAM also demonstrated predictive validity for outcome of treatment.
As discussed by Block, Gatchel, Deardorff, and Guyer (2003), the DRAM has been applied to presurgical psychological screening for spine surgery in chronic back pain patients. Trief et al. (2000) administered the DRAM to chronic back pain patients who ultimately underwent lumbar fusion. The DRAM was predictive of daily function, ability to sustain work-leisure activities, and change in back and leg pain after surgery with the Distress groups showing the worse outcomes. In two other studies the DRAM failed to find that distressed patients had a poorer outcome to posterior lumbar interbody fusion (Hobby et al., 2001) or lumbar discectomy (Tandon et al., 1999). However, the distressed groups did show less of a response to the surgery when compared to the Normal group, but these trends were not significant. The small sample sizes (N=fewer than 60) may have impacted these results.
Waddell’s Nonorganic Signs. Waddell (See Waddell, 1998 for a review) developed a physical examination technique as another method of assessing pain sensitivity (symptom amplification or pain beyond what would be expected due to objective findings). Waddell’s “test” includes five maneuvers completed by the physician as part of the physical examination including: nonanatomic tenderness, simulation tests, distraction, regional disturbances, and overreaction. In doing a pre-surgical screening, you may or may not have Waddell findings available since it is the physician’s responsibility to complete this test. In should be noted that the Waddell examination has proliferated in clinical practice as a test of malingering (purposeful feigning of illness) which is not accurate. It is a test of pain sensitivity and this does not imply volitional “faking” of symptoms on the part of the patient.
Depression
Major depression occurs frequently in patients with chronic spine pain (See Deardorff for a review) and has been found to predict poor spine surgery outcome in some studies but not in others (See Block et al, 2003 for a review). These inconsistent findings may be explained by the likelihood that there are actually subgroups of depressed patients. On the one hand are the patients that have protracted depressive symptoms (either antedating a chronic pain problem or associated with it). Given the chronicity of the depression, these patients may be less likely to have their psychological symptoms resolve after surgery. The other group might be conceptualized as those patients with reactive depression that is more acute and reactive to the pain. This sub-grouping has been substantiated in recent studies suggesting that spine pain patients with shorter duration of symptoms and lack of other psychosocial risk factors might show pre-operative depression in response to the pain (“reactive depression”) but this resolves after successful surgery (Block et al., 2003; Carragee et al., 2001; Hobby et al., 2001). If the MMPI-2, DRAM, BHI-2 or similar tests are used to assess pain sensitivity, a depression score is included in the test. Another rapid measure of depression is the Beck Depression Inventory-II (BDI-II).
Other Emotional and Cognitive Factors
Although depression is the most commonly assessed emotional predictive factor, other affective and cognitive states have also been investigated. It is beyond the scope of this discussion to review this extant literature. Block et al. (2003) discuss a pre-surgical screening method that was developed based upon Block’s prospective study (2001) of psychosocial variables that predicted spine surgery outcome. In his research, anger, anxiety and catastrophic thoughts were found to add predictive power to the regression equation. Anger was measured by Scale 4 of the MMPI (Pd), anxiety was measured by Scale 7 (Pt), and catastrophizing by the scale of the same name on the Coping Strategies Questionnaire (CSQ). The approach in this course provides the practitioner the flexibility to decide if and how to assess these other variables.
Millon Behavioral Medicine Diagnostic (MBMD). The MBMD is an updated version of the Millon Behavioral Health Inventory. The MBMD is a 165-item, true-false, self-report, instrument designed for the psychological assessment of adult medical patients (18 years or older, with 6th grade reading ability). The scales are grouped into five domains: Response Patterns (3 scales that help gauge distorted response tendencies in the patient's self-report), Negative Health Habits (5 scales that help gauge recent or current problematic behaviors affecting health, such as alcohol, drug, eating, caffeine, inactivity, and smoking), Psychiatric Indications (5 scales that help identify psychiatric comorbidities that may affect health management such as anxiety, depression, cognitive dysfunction, emotional liability, and guardedness), Coping Styles (11 scales that help identify patients' approaches to handling everyday problems, medical conditions and major life stressors), Stress Moderators (6 scales that help identify attitudes and resources that may affect health care), Treatment Prognostics (5 scales that help predict problems with treatment) and Management Guide (2 scales that help with treatment management).
As far as we know, the MBMD has not been specifically researched relative to its ability to predict clinical outcome to spine surgery. In one study, its predecessor (the MBHI), was assessed relative to its ability to predict lumbar laminectomy outcome compared to the MMPI (see bibliography) and it was found that the scales as a group were not associated with surgical outcome. Certain scale may provide useful information relative to the variables we have discussed. For example, these include the Negative Health Habits (Alcohol, Drugs, Inactivity, Smoking); Psychiatric Indicators (Anxiety, Depression); and, Stress Moderators (Illness Apprehension, Functional Deficits, Pain Sensitivity) Spousal Relationship
Research has determined that the spousal relationship can have a significant impact on the chronic pain patient’s recovery or lack thereof. In summary, problematic spousal responses to chronic pain that may be assessed as part of a pre-surgical screening can be classified as reinforcing or punishing the pain behaviors (for a more detailed discussion of this issue see Chronic Pain Management I: Concepts or QME Chronic Pain Management I: Concepts). Examples of a spouse (or family system) “rewarding” pain behavior might include such things as: (1) a spouse asking to rub her husband’s back when a groan is heard, (2) a spouse “knowing" when to bring pain medication even when her husband has not asked simply by knowing "the look on his face", and (3) warning the husband/patient not to "overdo it" when the spouse sees him slowly limping past.
Punishing responses occur when a spouse may express his or her anger toward the patient regarding the chronic pain (either directly or indirectly). Often, it is not socially acceptable to express anger directly towards the patient for all of the negative issues related to the pain and associated losses. Therefore, the spouse will do it indirectly by such things as ignoring the patient altogether, getting irritated frequently, or making comments about the patient’s character (e.g. “you’re not hurt that bad”, etc.). Block et al. (2001) found that spousal solicitousness and lack of support added to the power of the predictive equation. In the Block et al. (2001) study, these factors were assessed by interview. An additional method is to include a measure such as the Multidimensional Pain Inventory (MPI). The MPI includes scales of Support, Punishing Responses, and Solicitous Responses, all of which related to assessment of these relationship issues. In addition, other scale results can be used to corroborate the findings from other data sources. Multidimensional Pain Inventory (MPI). The MPI is a 56-item measure comprised of three sections. The first section includes items assessing: (1) pain severity and suffering; (2) interference of functioning due to pain; (3) perceived life control (4) affective distress; (5) support from spouse or significant other. The second section assesses the patient's perception of how much the spouse or significant other is displaying solicitous, distracting, or punishing responses to pain or suffering behavior. The third section assesses the patient's level of activity in areas of household chores, outdoor work, activities away from home, social activity and general activity level. The length of the MPI is well tolerated by patients, taking only about 15 to 20 minutes to complete.
The computer scoring generates a scaled T-score and classifies the case into one of three empirically derived prototypic profiles: "Dysfunctional" (high pain severity, affective distress, and life interference with low life control and activity levels); "Interpersonally Distressed" (low levels of support from significant others); and, "Adaptive Coper" (the opposite of Dysfunctional: low levels of pain severity, affective distress, and life interference with higher levels of life control and activity). The scoring software for the MPI can be purchased for 200 dollars and allows for unlimited uses (MPI Scoring Program).
The MPI was specifically developed for pain patient assessment. The standardization and normative data are all derived from populations of pain patients. The MPI is theoretically linked to a cognitive- behavioral perspective of chronic pain and health assessment. Because the MPI was developed for use with pain patients, the item is relevant to the experience of the person with chronic pain. Therefore, patients generally do not question why the questionnaire is being used to assess their problem.
The MPI was designed to be a brief measure of specific characteristics of pain patients. As such, it does not yield any detailed information about such things as depression, anxiety or somatization (the affective distress scale has questions and its content is related). It also is not designed to screen for psychopathology that might impact chronic pain treatment. Therefore, the MPI might be best used in conjunction with another instrument such as the SCL 9O-R or MMPI-2.
Psychiatric Treatment History
Psychiatric treatment history or “prior psychological problems” (Block et al., 2003) should be assessed as part of a pre-surgical screening. As discussed by Block et al. (2003), many patients with chronic pain will have psychological problems along with a treatment history. One goal of the clinical interview is to determine the temporal relationship of the psychological problems and the chronic pain. Many patients with chronic pain will present with significant psychological problems but absolutely no history prior to pain onset. This type of patient might be quite different then the individual who has had longstanding psychiatric problems with a marginal level of function even before the onset of pain. MEDICAL VARIABLES
Few studies have identified medical factors that are consistent and unequivocal predictors of poor spine surgery outcome. Of the predictive variables investigated (See Table 2), duration of symptoms, number of previous spine surgeries, and associated medical problems have reasonable support in the outcome studies and are most amenable to a presurgical screening.
Duration of symptoms. As discussed by Mannion and Elering (2005), “A consistent predictor of poor outcome for various different diagnoses and types of outcome is the duration of symptoms prior to the operation” (p.14). Duration of symptoms has been measured directly and as a component of other predictor variables (e.g. length of disability, workers’ compensation, sick leave) and the results are the same. Consistent with theories on the development of the chronic pain syndrome (see the chronic pain management courses), the longer duration of symptoms allows for other biopsychosocial issues to emerge that adversely impact spine surgery outcome (e.g. physical and mental deconditioning, psychological distress, etc.). As summarized by Block et al. (2003), “It appears, then, that time until surgery is the enemy of recovery, for as pain persists many adverse effects can accumulate, diminishing patients’ financial, emotional, and physical resources” (p. 44).
Number of previous spine surgeries. It is estimated that the failed back surgery syndrome occurs in 10% to 40% of all spine surgeries and the probability of good surgical outcome decreases with each successive surgical intervention (Block et al., 2003; Mannion and Elfering, 2005). However, there is evidence that patients who have responded well to a previous spine surgery are more likely to do better with additional surgery assuming a clear pain generator has been identified and is amenable to surgical intervention (Mannion and Elfering, 2005 for a review). Even so, the number of previous spine surgeries, especially when one gets into the realm of “salvage” spine surgery, is certainly a predictive variable that should be evaluated.
Associated medical problems. This predictive variable category is assessed by evaluating prior medical utilization and co-morbid health conditions. A myriad of studies have demonstrated diminished spine surgery outcomes in patients with a history of many prior illnesses and non-spine surgeries. This may be due to the fact that prior medical utilization reflects sensitivity not only to pain but also to physical symptoms in general. Co-morbid medical conditions and poor general health might impact spine surgery outcome due to such things as problems with wound healing (e.g. with diabetes) or post-operative rehabilitation (e.g. with other joint problems or systemic issues such as fibromyalgia).
Type of surgery. The type of surgery should be considered as part of a pre-surgical screening taking into account not only the extensiveness of the procedure but also the patient’s ability to manage the recovery. As discussed by Mannion and Elfering (2005), the number of affected levels is often assumed to be inversely related to outcome. Studies have shown this inverse relationship (more levels greater risk) for disability status after fusion, long-term clinical outcome after laminectomy, and the risk of requiring subsequent fusion after discectomy. However, other studies have not established this relationship. It may be that accurately identifying the correct surgically treatable lesion(s) may be of the utmost importance. As discussed by Mannion and Elfering (2005) and others, increasingly poor results can be expected when more levels are wrongly operated.
Related to this issue is the type of surgery beyond the number of levels operated. For instance, a simple single level laminectomy is a much different procedure than an anterior-posterior two level fusion. These differences should be taken into account as part of a comprehensive pre-surgical screening. ADVERSE CLINICAL FEATURES
Block et al. (2003, p 107) has identified adverse clinical features that should also be assessed as part of a pre-surgical screening. These can be found in Table 15.
SUMMARY OF PRE-SURGICAL SCREENING VARIABLES
Table 16 is a summary of the pre-surgical screening variables reviewed in this course and the associated method of evaluating these risk factors. It should be noted that this list of risk factors is by no means exhaustive. In addition, the example data sources are only suggestions. This list is not to imply that every patient should be administered all of these psychological tests. The approach presented in this course allows the clinician flexibility in choosing how each variable is evaluated. Often, a clinical interview is completed and then the test battery modified as appropriate (e.g. the police officer who had a work injury, continues to work with his symptoms, takes no medication, loves his job, shows no risk factors in the clinical interview, and is scheduled to undergo a microdiscectomy may not need the entire PSS battery of tests).
INTRODUCTION TO THE CASE EXAMPLE
We have reviewed a number of variables that can be assessed as part of a pre-surgical screening (PSS). As discussed, a number of methods and decision-rules have been developed relative to PSS. Probably the most comprehensive is the work of Block et al. (2001, 2003), in which a group of patients (N=204) who were scheduled to undergo laminectomy/diskectomy or spinal fusions underwent a PSS consisting of a semi-structured clinical and psychological testing. The surgeons were blind to the results of the PSS and the patients were assessed for outcome at approximately 6 months post-operative. Based upon the statistical analyses, a “scorecard” approach was developed (e.g. Total Psychosocial Risk Factors rated 0-8 or more; Total Medical Risk Factors rated at 0-6 or more, etc.). Very specific decision rules were developed that places patients into one of five categories: Good Prognosis-No psych treatment, Good Prognosis-Postoperative psych treatment, Fair Prognosis-Address preoperative issues, Poor Prognosis-Noninvasive treatment recommended, and Poor Prognosis- Discharge recommended (See Block et al., 2003 for a detailed outline of this method).
The following case example evaluation report will present a method that is based upon Block et al. (2003) but does not use the scorecard approach or exactly the same measures. The goal is to assess each Risk Factor and then develop a recommendation based upon the findings. You will notice with I like to use a convergent-validity type of approach. The evaluation rarely relies upon one data source to count it as “positive”. Rather, I believe it is important to look for data convergence. When discrepancies exist, these should be explored by the clinician until he or she is satisfied that the Risk Factor has been validly assessed.
The following is a hypothetical pre-surgical screening based upon a conglomeration of several cases I have evaluated. I chose to include a vast number of risk factors for illustrative purposes. This case represents a worst case scenario in terms of a patient heading towards spine surgery. As will be seen, it was recommended that the patient avoid spine surgery and alternative treatments were recommended. In training behavioral health practitioners to complete PSS evaluations, I have noticed there is a reluctance to screen a patient out in terms of getting the elective surgery. It appears they are concerned about “going against” the recommendation of the surgeon and his or her medical opinion. Remember, you are making a statement about the probability of a clinical success in response to an elective spine surgery directed primarily at pain relief and function. If the evaluation is done properly, the variables you are assessing are more powerful predictors of outcome than the physical data assessed by the surgeon. After stating your professional opinions (e.g. clear, not cleared, etc.), it will be incumbent on the surgeon to take them into account. I have had many cases in which the surgeon agrees and no surgery is offered. Unfortunately, I have had an equal number of cases in which the surgeon simply goes ahead with the surgery regardless of the PSS results (assuming he or she can get insurance approval given my findings and the patient is agreeable). In the vast majority of these latter cases, I will be seeing the patient again at about one year post-operative for chronic pain management and the Failed Spine Surgery Syndrome.
Presurgical Psychological Screening and Pain Evaluation
Patient Name: Jane Smith Referring Physician: Dr. Algology Date of Evaluation: Claims Examiner: Date of Injury: Applicant Attorney: Defense Attorney: Employer: Claim Number:
Procedures Used: Comprehensive Clinical Interview Pre-Surgical Psychological Assessments of: Pain and Functional Ratings Patient Pain Drawing MMPI-2 Battery for Health Improvement-2 Pain Patient Questionnaire Multi Dimensional Pain Inventory Modified Somatic Perceptions Questionnaire Beck Depression Inventory-2 Review of Available Medical Records
Purpose of Consultation. Consistent with the ACOEM Practice Guidelines, this patient has been referred for assessment of a chronic pain and disability syndrome. This type of condition is described in the Practice Guidelines (ACOEM, 2004) as System-Induced Functional Disability (pages 87-88) and Delayed Recovery Associated with Chronic Pain (chapter 6, pages 105-126). The purpose of this consultation was to determine this individual’s psychological and mental status and whether significant psychological and behavioral factors are contributing to the pain and disability.
In addition, in cases of cervical and/or lumbar spine surgery, the Occupational Medicine Practice Guidelines (ACOEM, 2004) underscore that psychological screening for spine surgery should be considered. In cervical surgery the Practice Guidelines state that, “If surgery is a consideration, counseling and discussion regarding likely outcomes, risks and benefits, and especially expectations is essential (ACOEM, 2004, p. 180). It goes on to state that, “Pre-surgical screening should include consideration of psychological evaluation” (p. 181). In lumbar spine surgery, the Practice Guidelines state that, “Before referral for surgery, clinicians should consider referral for psychological screening to improve surgical outcome…..” (p. 306). The Practice Guidelines support these recommendations by concluding, “Social, economic, and psychological factors can alter a patient’s response to symptoms and treatment such as spinal surgery” (p. 310).
Pre-surgical Screening (PSS) can identify cases that are likely to be a “technical success but clinical failure” (Block, Gatchel, Deardorff & Guyer, 2003; Block, 1996; Deardorff, 2000). This is due to the fact that psychosocial and non-physical factors are generally stronger predictors of clinical outcome than physical findings (See Block et al., 2003 for a review). The PSS evaluation is comprehensive and assesses variables that have been shown to negatively impact surgical outcome.
Identifying Information:
This is a 45-year-old single female who sustained multiple industrial injuries during the course of her employment with Smart Kids College Preparatory Academy.
Presenting Problem and Review of Available Medical Records:
Obtaining a detailed and focused history from the patient was difficult since she was a relatively poor historian for events. Therefore, the following relies not only on the patient’s self-report during the clinical interview, but also a review of copious medical records. Given the patient’s extensive medical history since the injury, and the fact that she has suffered multiple injuries, only those medical records relevant to the current evaluation will be discussed in detail.
The patient reported that on 12/10/2004 she was performing her usual job duties as a custodian when she was injured. She was standing on a ladder, reaching up and cleaning a fan, when her “back went out” and she experienced immediate onset of pain in the low back region. She reported the incident to her employer and was sent to an Occupational Medicine Clinic for evaluation and treatment. The patient was taken off of work and started on a course of conservative treatment including medications and physical therapy. This was completed for approximately two months.
After the injury of 12/10/2004 the patient continued to complain of low back and right leg pain. Medical records indicate the patient’s attorney referred her to an orthopedic surgeon, Dr. Lami. She was initially evaluated by Dr. Lami on 12/23/2004. An MRI of the lumbar spine was ordered along with electrodiagnostic studies of the bilateral lower extremities.
The patient underwent the lumbar MRI on 1/11/2005. Medical records indicate diagnostic impressions included a 2 mm posterior disc protrusion at L3-4, a 2 mm posterior disc protrusion at L4-5 with disc dessication, and a 2-3 mm posterior disc protrusion at L5-S1 with disc dessication and mild bilateral hypertrophic facet changes.
The patient underwent electrodiagnostic studies on 1/14/2005. The findings were consistent with left L5 radiculopathy. Medical records indicate this is inconsistent with her subjective complaints of right leg pain.
According to the patient and medical records, Dr. Lami started her on a course of physical therapy which was beneficial. In fact, during the course of the clinical interview, she stated that the physical reactivation oriented and strengthening physical therapy prescribed by Dr. Lami was “the only thing that has ever helped me.” She stated she desired to continue the treatment, but it was discontinued due to lack of authorization.
Medical records indicate that Dr. Lami referred the patient to a medical pain management specialist, Dr. Disruption in June of 2005. The patient was placed on various medications and a series of lumbar epidural steroid injections was completed. The patient reported these were not beneficial.
The patient remained under the care of Dr. Lami and Dr. Disruption for quite some time. Ultimately, she was sent to Dr. Algology for an orthopedic AME on 5/12/2006. The patient reported her last day of work was 12/20/04. The evaluation notes that she presented with what appeared to be right-sided radiculopathy “as judged by the probable presence of some right thigh atrophy and right-sided S1 sensory deficit.” Dr. Algology noted that her MRI of 1/11/2005 “did not show much, other than some minor bulges.” He ordered an updated MRI and electrodiagnostic studies. He also felt that it was highly probable that she was permanent and stationary.
The patient underwent the lumbar MRI on 8/11/2006, “which showed no abnormalities.” She also underwent the electrodiagnostic studies at that time and these were considered “normal.”
The patient returned to see Dr. Algology on 9/8/2006. At that time, the MRI and electrodiagnostic studies were reviewed. Dr. Algology felt the patient was permanent and stationary and “there was no need for surgery.” Subsequently, she continued with routine follow-up visits with Dr. Feelgood.
Medical records indicate the patient was evaluated by Dr. Gas on 12/19/2008. The report documents that the patient had not worked since 12/10/04. The report also documents that the patient submitted paperwork for early retirement in 2005 due to her back pain. The report documents that the patient was complaining of significant pain in the upper and mid to low back, radiating to the right leg and to her foot. She was also complaining of anxiety, stress, and depression. Dr. Gas felt the patient’s condition remained permanent and stationary.
Medical records indicate that the patient underwent a lumbar discogram completed by Dr. Needle in either June or August of 2008. Findings included a negative discogram at L3-4 and L4-5. The discogram was evidently positive at L5-S1 with “moderately severe to severe pain.” The pain was “full concordant.” In this report, it is evidently documented that the concordant pain was in the low back and left leg. Of course, this is inconsistent with her subjective complaints and symptoms as reported elsewhere.
Medical records indicate that the patient continued to follow-up with Dr. Feelgood on a regular basis. As of 1/16/2009, the patient was complaining of increasing low back and leg pain. He was continuing to recommend an artificial disc replacement at the L5-S1 level. He placed the patient on TTD.
Medical records indicate that Dr. Feelgood again requested authorization for the artificial disc replacement at L5-S1 on 1/31/2009. This was denied by Utilization Review on 2/8/2009. Dr. Feelgood reevaluated the patient on 2/13/2009. He continued to recommend the artificial disc replacement. The progress note states he cited a positive MRI and discogram at L4-5 and L5-S1 levels. This is inconsistent with the medical records indicating a positive discogram only at L5-S1.
The patient was sent back to Dr. Algology for reevaluation on 6/23/2009. At the time of the evaluation, the patient was rating her low back pain at an 8/10 “which is present most of the time.” She stated her pain at the time of the evaluation was a “10.” She reported that the low back pain radiates down the right leg and that she will limp as a result. She rated her right lower extremity pain at a 7/10. The patient was also complaining of neck pain and right arm pain localized at the elbow. Medications at that time included Naprosyn, Lorazepam, Hydrocodone, Orphenadrine, Wellbutrin, Buspar, Seroquel, and Temazepam. The patient reported she smokes one pack of cigarettes per day and consumed one beer per day. Dr. Algology noted that the medical records did not show a complete chronology of treatment from 2004, but started again in 2006. Dr. Algology presented a lengthy discussion relative to the conflicting diagnostic findings (e.g. Dr. Needle reported left leg pain when the patient has consistently reported right leg pain, the MRI findings are on the left side while the patient’s symptoms are on the right side, etc.). Dr. Algology suggested a presurgical psychological screening consistent with ACOEM Practice Guidelines and evidence-based literature. Dr. Algology also disagreed with Dr. Feelgood relative to the permanent and stationary versus TTD issue. Dr. Algology felt that the patient had a “fairly significant chronic pain problem,” but “it represents more or less a benign pain problem.” He felt that Ms. Smith was not currently a candidate for surgery, but it was possible pending the presurgical psychological screening and resolution of the contradictory discogram findings.
During the course of the clinical interview, the patient stated that she has been treating with Dr. Feelgood “for about two years.” She expressed frustration with the treatment stating “he has only given me medications.” She also stated he has never “touched me, examined me or nothing.” She follows-up with Dr. Feelgood about every four weeks. She stated “I am tired of it,” and “he doesn’t treat me.” She also felt that Dr. Feelgood “was not happy with me.” Dr. Feelgood has recommended the artificial disc replacement at L5-S1. The patient’s understanding of his recommendations will be discussed under a subsequent section “expectations regarding surgery.”
Since the AME Reevaluation of Dr. Algology on 6/23/2009 the patient was hospitalized on a psychiatric and involuntary basis. The patient reported that she took an overdose of Temazepam on 9/15/2009 in the evening. The patient had written “goodbye notes” to several friends and relatives. The patient reported that she did awaken the following morning and contacted her psychiatrist, Dr. Mesmerized. According to the patient, Dr. Mesmerized had her come to the office for evaluation and was immediately sent to the emergency room. She was evaluated and taken by ambulance to the ER. She was admitted on 9/16/2009.
The copious medical records from her psychiatric hospitalization were reviewed. The psychiatric emergency team evaluation of 9/16/2009 indicates the patient had attempted to overdose on the Temazepam the prior evening. She was complaining of anxiety, depression, and stress. The report indicates that she had not eaten for five days. Stressors included being evicted from her apartment, “herniated disc,” and ongoing lawsuit. The patient had been prescribed Seroquel, but was “not medication compliant.” The intake report also indicated she regularly consumed alcohol while taking her psychotropic medications. She reported drinking 16 ounces of beer on a daily basis with her sleeping medications. She had also used marijuana within the last week. The admitting diagnosis included rule out major depression, severe, without psychosis; and, anorexia nervosa. The patient was determined to be a danger to herself and placed on a 72 hour involuntary hold. The toxicology screen was positive for cocaine and the patient stated she had “a little cocaine before my hospitalization.”
The patient was hospitalized for approximately five days and discharged on 9/22/2009. Medical records indicate that she underwent various treatments while hospitalized including medication changes, as well as individual and group psychotherapy treatment. The hospital medical records are conspicuous for lack of any complaints relative to pain or request for pain medications. The patient was admitted with a GAF of 20 which is extremely low. She was discharged with a GAF of 45. The patient was discharged to home with the recommendation for individual psychotherapy follow-up visits on an outpatient basis, chemical dependency treatment, and psychopharmacology treatment. Her discharge medications included Prozac and Seroquel.
Current Symptoms and Level of Function:
The patient stated that her current symptoms include pain in the low back with radiation to the right leg. She stated that her pain is primarily in the low back and right hip. The patient’s current typical day includes getting up between 8:30-9:00 a.m. She will have breakfast and engage in light ADLs around the house “if I feel good.” The patient tends to spend most of her time at home and is “up and down all day.”
Work History:
The patient reported she began working for Smart Kids Academy in 1991 and her last day of work was in December of 2004. The patient stated that she was medically retired at that time. The patient worked as a custodian.
Other Medical Problems:
The patient stated that she is “fairly healthy” aside from the chronic pain and psychiatric issues. She stated that although the hospital diagnosed some type of eating disorder, “I have always been thin.”
History of Work Injuries:
Aside from the three work injuries already reviewed, the patient denied any history of other work injuries.
Surgical History:
The patient reported she has had fairly minor surgeries in the past requiring a one night stay in the hospital. She stated these surgeries were for “fibroid tumors.”
Interviewer Observations and Mental Status Examination:
The following is a summary of interviewer observation and a mini-mental status examination. A formal mental status examination was not necessary.
Attitude: The patient was open and cooperative during the course of the clinical interview, but getting a history was somewhat difficult. Pain Behaviors: The patient did not display any pain behaviors during the extensive clinical interview. Mood/Affect: The patient described her mood as “battling depression and anxiety daily.” When discussing her depression, anxiety, and psychiatric treatment history, the patient began to become quite tearful. She also stated “I am having a panic attack.” The patient paused during the interview and completed some deep breathing exercises while closing her eyes. After a short time, her anxiety episode subsided and we continued with the interview. Aside from this instance, the patient’s affect was actually fairly bright. Crying Spells: The patient reported experiencing spontaneous crying spells approximately twice per week. Sleep: The patient reported her sleep is “still bad” including difficulty falling asleep and awakening during the night. She will occasionally nap during the day. Appetite and weight changes: The patient reported her weight has been stable since increasing weight during her hospitalization. She believes she now weighs between 90 and 95 pounds. She reported that this is “normal” for her. Energy level: “A little better.” Memory and concentration abilities: The patient reported she has some trouble with memory and concentration, especially when “stressed.” Suicidal ideation, plan, previous attempts: The patient did make a suicide attempt by overdose as discussed previously. This occurred on 9/15/2008. The attempt seemed to be fairly significant since the patient lives alone, she took the medications in the evening, and she did leave letters for family and relatives. The review of her psychiatric hospitalization has been discussed previously. During the course of the clinical interview, the patient tended to downplay the seriousness of her suicide attempt. She stated that it was a suicide attempt, but she was “really tired” and “just wanted to sleep.” The patient currently denies any type of suicidal ideation or formulated plan. She denies any history of other suicide attempts. Sexual functioning: The patient is not currently in a relationship and is not sexually active. Symptoms of generalized anxiety or panic: The patient reported that she does suffer from generalized anxiety and occasional panic attacks. Thought Process: The patient showed no evidence of a thought disorder. Orientation: The patient presented with a clear sensorium and was oriented in all spheres.
Psychosocial Situation:
The patient’s parents are both deceased. Her mother died approximately three to four years ago. The patient has never been married. She does have a 28-year-old daughter with whom she has had no contact in five or six years.
The patient has two half-brothers ages 44 and 55-years-old and two sisters ages 40 and 42 years old. She stated that she has no contact with any of her siblings for approximately 10 years. One sister and one brother are possibly schizophrenic.
The patient currently lives alone. Her social network includes “one or two friends.” The patient stated that she drives short distances. Distractive and recreational activities currently include “going out to eat with a girlfriend.” The patient previously enjoyed fishing, walking, and gardening. She no longer engages in these activities. She also previously engaged in a regular exercise program. She stated it was quite helpful with her depression, stress, and pain. She currently engages in no exercise activity.
It should be noted that the psychiatric hospital records indicated the patient had a niece who is on Seroquel and her daughter had her placed on a psychiatric hold through Kaiser Mental Health Center at some point in the past.
Early Childhood Development:
The patient described her early childhood as “okay” and “happy.” She specifically denied any history of physical, emotional, or sexual abuse.
Psychiatric Treatment History:
The patient reported a long history of psychiatric and psychological treatment. Medical records indicate she was treated by Dr. Freud, a psychiatrist beginning in 2001 on an industrial basis. The course of treatment including psychotherapy lasted at least three years. Subsequently, she came under the care of Dr. Mesmerized, a psychiatrist, who placed her on TTD. She treated with him, including psychopharmacology and psychotherapy, for approximately three years. Subsequently, the patient came under the care of a different Dr. Mesmerized, a psychiatrist at Kaiser. She has treated with him for the past six years.
Since being discharged from the psychiatric hospital, the patient is no longer treating with her psychiatrist, Dr. Mesmerized. The patient has tried more than one psychotherapist since her discharge.
The patient has not seen a psychiatrist since her discharge from the hospital. She stated this was due to financial issues. The patient stated that she could not afford the co-pay for treatment visits provided through Kaiser
Substance Use:
The patient denied any history for treatment for substance abuse or chemical dependency problems. However, she did report cocaine use just prior to her psychiatric hospitalization. She denied any cocaine use since that time. The patient states she currently “smokes a little marijuana” to help with her appetite. The patient stated that she previously “used to drink hard liquor.” The patient currently reports drinking a 16 ounce beer in the evenings. Her report varied from once or twice per week to every evening. On the Pain Patient Questionnaire, the patient stated she consumes two 12 ounce cans of beer per day. The patient denied the use of any other illicit or recreational substances. In addition, the patient has smoked one pack of cigarettes per day for the past 38 years. The patient reported drinking one cup of coffee per day and six colas per day.
Medications
Medications are reported to include Naprosyn, Lorazepam, Hydrocodone (up to 6 Norco per day), Wellbutrin and Buspar. Pain and Presurgical Tests:
The ACOEM Practice Guidelines (2004) suggest that psychological assessment should be carried out in the evaluation of chronic pain (page 115) and that pain assessment tools may also be useful (pages 125-126). As such, the patient was administered the assessment instruments listed previously. The following results were obtained:
Pain and Functional Ratings: On the Pain Patient Questionnaire, the patient rated her pain (0-100) at a 99, at its highest intensity, a 98 at its usual intensity, and a 90 at its lowest intensity.
Pain Drawing: On the Pain Drawing, the patient showed diffuse areas of pain along with using color (not specified in the instructions). The pain drawing is considered abnormal.
MMPI-2: The MMPI-2 is the most widely used psychometric instrument for presurgical screening prior to spine surgery. Numerous studies have demonstrated a relationship between MMPI-2 results and clinical outcomes to spine surgery. The results of the MMPI-2 are as follows:
Analysis of the consistency of item endorsement was evaluated using decision rules developed by Green (1991), and Pope, Butcher, and Seelan (2000, 2006) and others (see references). There were two item omissions which is within acceptable limits. The VRIN (T=70) was in the range suggesting the possibility of inconsistent responding. Careless responding can produce a VRIN in this range. The TRIN (T=65F) was also slightly elevated. TRIN scores in this range are suspect and also suggest the possibility of inconsistent responding. According to Pope et al. (2006), scores in this range indicate a response bias towards “yea-saying,” which is a tendency towards endorsing items inconsistently in the positive direction. Based upon these findings, it is concluded that the patient answered the items with a slight bias towards “yea-saying” but not enough to invalidate the clinical profile.
Validity of the profile was assessed using accepted standards. The patient demonstrated moderate elevations on F and Fb which reflects acknowledgement of unusual experiences and moderate distress. The patient did not show elevations on Scales L, K, S.
The Clinical Profile was interpreted relative to the chronic pain and presurgical screening issues. The patient produced a grossly abnormal profile. For presurgical screening, the most important scales are 1, 2, and 3, according to the evidenced-based research (see references). Also, for presurgical screening issues, a significant elevation on these scales is set at T=70 rather than the usual T=65. As can be seen, the patient demonstrated elevations beyond T=70 (Scales 1, 2, and 3).
As can be seen from the T-score values, the patient produced a grossly abnormal MMPI-2 Profile with very significant elevations on Scales 1, 2, 3, 4, 6, 7, and 8. According to Fordyce (See references), patients with similar profiles present with a wide variety of vague and diffuse somatic complaints and there is often a low correlation between subjective and objective findings. In addition, patients with similar profiles show a high level of “pain sensitivity” or “symptom amplification” which is defined as pain behaviors far beyond what would be expected due to nociceptive input. This suggests a significant contribution of non-physical factors (cognitive, affective, and operant) to the patient’s perception of pain, pain behaviors, level of suffering, and level of disability.
According to Fordyce, patients with this profile (elevations on Scales 1, 2, 3, and 4); typically describe a passive dependent person, who has considerable readiness to seek nurturance and support from others. These individuals may use pain behaviors to help obtain support and shelter from responsibility demands. For these individuals, pain/illness may not have a high response cost.
Patients with similar profiles often complain of problems with concentration and thinking. They are likely to be experiencing significant psychological distress despite their attempts to deny and repress problems. Psychological distress is converted into physical symptoms which may consist of bizarre complaints. They display histrionic features as well as hostility, tension, and worry. They may experience psychotic episodes.
As discussed by Block, Gatchel, Deardorff, and Guyer (2003, page 83), elevations on Scales 1 and 3 reflect excessive sensitivity to pain rather than the cause of the pain. In other words, in the face of a certain level of nociception, individuals who have high scores on Scales 1 and 3 are more likely to experience high pain levels, and to be more functionally disabled than those with low scores on these scales. As such, pain sensitivity, as assessed by Scales 1 and 3, seems to predispose patients towards negative spine surgery results even when the surgery corrects the underlying pathology (Block et. al., 2003, page 84). Individuals with this profile tend to respond very poorly to interventional and invasive pain management techniques aimed at identifying and “fixing” a physical pain generator. The reason they do so poorly is that the other non-physical factors continue to impact their perception of pain and suffering.
Battery for Health Improvement-2: The BHI-2 is a comprehensive self-report instrument designed for the psychosocial assessment of medical patients (Bruns & Disorbio, 2003). The purpose of the test is to provide assessment information and treatment recommendations for injured patients in a variety of settings. The scales of the BHI-2 have been found to correlate significantly with the MMPI-2. The BHI-2 assesses a number of areas relevant to the injured worker that are not assessed with the MMPI-2.
The patient did not endorse any of the validity items. This reduces the risk that this profile was produced by random responding. Patients with this profile are exhibiting an usually low level of Subtle Defensive Tendencies which was seen in only 11% of the Patient Standardization Group. Lowering of defenses tends to be associated with a heightened report of negative information. Patients with this profile type are reporting that their life circumstances are unusually difficult.
As can be seen, the patient produced elevations across all of the Physical Symptom Scales. This includes Somatic Complaints (extremely high), Pain Complaints (very high), Functional Complaints (extremely high), and Muscular Bracing (moderately high). According to the test interpretation manual, extremely high scores on the Somatic Complaints Scale suggests the presence of a very unusual level of diffuse Somatic Complaints. The higher the score, the less likely it is that any single organic condition can explain the reported pattern of symptoms. If there is no clear medical explanation for the patient’s pervasive pattern of Somatic Symptoms, the possibility of somatization is strongly indicated. Similarly, a very high score on the Pain Complaints Scale, without objective medical findings to explain the patient’s pain reports, suggest the possibility of a Somatoform Pain Disorder. Patients with extremely high scores on Functional Complaints tend to perceive themselves as being disabled in a broad range of functions and activities. The elevations on these scales suggest a high level of Symptom Amplification which is defined as pain behaviors far beyond what would be expected due to nociceptive input and objective findings. It also suggests that pain behaviors and overall level of suffering are being significantly impacted by non-physical factors. These results are consistent with the MMPI-2 results.
The patient scored moderately high on Depression. She also scored slightly below average on Perseverance. A low score on Perseverance is a poor prognostic sign relative to recovery from spine surgery.
The patient showed elevations on all of the Psychosocial Scales and this is consistent with her history.
Analysis of the Content Scales demonstrates that the patient scored very high across all of the Physical Symptom Content areas. The patient also scored high on Suicidal Ideation.
Multi-Dimensional Pain Inventory: This is a comprehensive self-report instrument that evaluates the impact of diverse chronic pain syndromes on multiple dimensions of a patient’s life (Turk and Melzak, 1992). The T-scores for each scale are as follows:
On the MPI, Cluster Classification was not possible since the patient does not have a significant other. As can be seen, the patient scored well above average for Pain Severity, Interference With Functioning, and Affective Distress. She scored well below average for Life Control. This suggests that the patient has a low level of self-efficacy relative to her current situation.
As can be seen, the patient scored well below average across all of the Activity Scales. This does suggest a fairly significant physical deactivation and deconditioning syndrome. This is consistent with what she described during the clinical interview.
Modified Somatic Perceptions Questionnaire: On the MSPQ, the patient scored a 25, which is in the very high range of somatic anxiety and somatic focus. This suggests that pain behaviors and overall level of suffering are being significantly impacted by non-physical factors (cognitive, affective, and operant).
Beck Depression Inventory-2: On the BDI-2, the patient scored a 52, which is in the severe range of self-rated depression.
Expectations Regarding Surgery:
When asked about her understanding of her lumbar spine condition, she stated “I have three herniated discs.” She reported that Dr. Feelgood essentially refused to explain the proposed surgical procedure. She also stated that she rarely actually sees Dr. Feelgood, but primarily is seen by the physician’s assistant. In summary, the patient stated “I have no idea what he wants to do.” She also stated that “the only thing I was told is that he will go through my belly button push my guts aside” to do the surgery. When discussing this issue, she stated “I would rather not go under the knife.”
Presurgical Screening Results:
Pre-surgical Screening (PSS). The comprehensive PSS was conducted consistent with the ACOEM Practice Guidelines and those established in research studies completed over the past 30 years. Most PSS systems assess variables across several dimensions: Biologic-Lifestyle Risk Factors, Pain Related Risk Factors, Psychosocial Risk Factors, Surgery and Medical Risk Factors and Adverse Clinical Features. All of the following risk factors have been demonstrated in the research as being related to a poorer clinical outcome to surgery. Those not specifically discussed were found to be non-contributory.
Biologic-Lifestyle Risk Factors
Cigarette Use - Positive
Active and Untreated Substance Abuse Disorder -Positive
The patient’s report of substances varies across different sources of evaluation data and medical records. During the course of the clinical interview, she originally stated that she is drinking approximately 16 ounces of beer each evening. She then recanted and stated this occurred only once or twice per week. On the Pain Patient Questionnaire, she reported drinking two 12 ounce cans of beer each evening. The medical records related to her psychiatric hospitalization indicate she was drinking beer each evening along with using marijuana and cocaine. Given the research on self-report of substance use, it is likely that the higher estimates of alcohol use are more accurate. Therefore, current substances would include alcohol and marijuana. The patient reported she has not used cocaine since her hospitalization.
Obesity - Negative
Exercise and Activity Level - Positive
The patient shows physical deactivation as evidenced by the MPI Activity Scales and the clinical interview.
Work-Related Risk Factors:
Workers Compensation- Positive
Pain Related Disability/Litigation- Positive
Not Work Greater Than Six Months – Positive
Job Dissatisfaction- Positive
Psychological Risk Factors:
Pain Sensitivity/Symptom Amplification - Positive
Pain sensitivity and symptom amplification are defined as pain behaviors beyond what would be expected due to nociceptive input and objective findings. Clearly, Dr. Algology had concerns regarding the patient’s pain behaviors given her minimal findings on the imaging studies. The psychological testing battery substantiates this opinion and suggests that the patient’s overall level of pain perception and suffering is being significantly impacted by non-physical factors (cognitive, affective, and operant). Symptom amplification and pain sensitivity are documented on the MMPI-2, BHI-2 (Somatic Complaints, Symptom Dependency) and the MSPQ.
Medication Seeking Behavior – Negative (Possibly Positive)
Major Chronic Pain Syndrome - Positive
This patient clearly shows multiple aspects of a significant chronic pain syndrome. These include physical and mental deconditioning as conceptualized by Gatchel (2004), concomitant depression and anxiety including panic attacks, sleep disruption, diminished self-efficacy, social isolation, and pain related disability. In these cases, simply repairing a pain generator causing nociceptive input (assuming it has been accurately identified) often has no effect on the actual chronic pain syndrome symptoms.
Abnormal Pain Ratings - Positive
On the Pain Patient Questionnaire, the patient rated her pain (0-100) at a 99, at its highest intensity, a 98 at its usual intensity, and a 90 at its lowest intensity. This pattern of ratings demonstrates a significant lack of variability.
Abnormal Pain Drawing - Positive
Major Uncontrolled Depression and/or Anxiety - Positive
The patient presented herself as well kempt, pleasant, talkative, and with a fairly bright affect during the course of the clinical interview. However, she was easily brought to tears when beginning to discuss her depression, anxiety, panic attacks, and recent psychiatric hospitalization. The patient also experienced a mild anxiety attack during this discussion. As such, one might conclude that her depression and anxiety is somewhat uncontrolled and easily triggered by stressful stimuli. In addition, the patient has not yet seen her new psychiatrist and may not be reasonably stabilized on her psychotropic medication regimen.
Unresolved Psychiatric Co-Morbidity - Positive
As discussed previously, the patient does have unresolved psychiatric issues. She is just now beginning treatment with a marriage and family counselor and psychiatrist.
Active Suicidal or Homicidal Behavior - Negative
Pre-Injury Psychiatric History - Positive
Serious Cognitive Deficits - Negative
Sleep Disturbance - Positive
Lack of Social Support - Positive
The patient stated her current social support network includes “one or two close friends.” The patient has had no contact with any family members for at least five years. The patient previously attended church on a regular basis, but has not done so for quite some time. Therefore, social support is minimal.
Spousal Solicitousness/No Support - N/A
History of Abuse/Abandonment - Negative
Medical and Surgery Related Factors:
Previous Spine Surgery - Negative
Proposed Surgery is Extensive - Positive
Non-Spine Medical Problems - Negative
Lack of Understanding of Procedures - Positive
The patient’s lack of understanding regarding the proposed surgery is of great concern. When asked about her understanding of her lumbar spine condition, she stated “I have three herniated discs.” She reported that Dr. Feelgood essentially refused to explain the proposed surgical procedure. She also stated that she rarely actually sees Dr. Feelgood, but primarily is seen by “Dr. Mesmerized.” Dr. Mesmerized may actually be a physician’s assistant. In summary, the patient stated “I have no idea what he wants to do.” She also stated that “the only thing I was told is that he will go through my belly button push my guts aside” to do the surgery. When discussing this issue, she stated “I would rather not go under the knife.”
Other Adverse Clinical Features:
Impulse control problems - Positive
The patient clearly has impulse control problems as demonstrated by her suicide attempt last year. She may also demonstrate impulse control problems related to her use of substances.
Treatment Compliance Issues - Positive
There are several issues related to treatment compliance as evidenced by the process of evaluation and the review of medical records. Relative to the evaluation, the patient was rescheduled one week later from her original appointment date. This is understandable if she was having transportation problems. After being told to arrive at least one hour prior to the appointment, she arrived 25 minutes late. Subsequently, after being told she must complete all of the presurgical screening questionnaires in the office, she failed to complete the MMPI-2. She offered no explanation and simply left the office. She had to be reschedule one week later to complete the MMPI-2
Distress and risk assessment method (DRAM):
The Distress and Risk Assessment Method. In addition to the PSS protocol, the Distress and Risk Assessment Method (DRAM; Main, 1983; Main, Wood, et al., 1992) was also used as an additional pre-screening evaluation. The results of the DRAM Screening for Ms. Smith places her in the Distressed-Somatic Category suggesting a poor prognosis for responding to a spine surgery. As such, according to the DRAM system, the patient was not cleared for surgery as well. This was a combination of the results of the MSPQ (25) and the Beck Depression Inventory (52).
Results of the Presurgical Screening (PSS) and DRAM:
Based upon the PSS and DRAM data, Ms. Smith is placed in the “poor prognosis” category in both systems relative to undergoing the proposed spine surgery at this time. In these cases, the PSS identifies a myriad of biopsychosocial factors that would preclude a successful clinical outcome to a spine surgery. Impressions and Conclusions:
Purpose of Evaluation. The presurgical screening addresses two questions:
Are there significant biopsychosocial factors that would preclude a successful clinical response to the surgery?
Is the patient at significant risk for psychiatric decompensation as a result of proceeding with an elective spine surgery?
Chronic Pain Syndrome and Symptom Amplification. The patient demonstrates a chronic pain and disability syndrome along with significant symptom amplification (See results of testing battery and other clinical data), suffering and emotionality. Symptom amplification is defined as pain behaviors beyond what would be expected due to nociceptive input, physical and objective findings. Symptom amplification occurs as part of a chronic pain and disability syndrome and is due to the contribution of non-physical factors (cognitive, affective, and operant/behavioral) to the individual’s level of pain perception and overall level of suffering. In these cases, surgical decision-making cannot simply be guided by the patient’s report of pain.
Risk of Poor Clinical Outcome. This assessment answers the question: Are there significant biopsychosocial factors that would preclude a successful clinical response to the surgery?
The biopsychosocial evaluation of risk factors suggests that this patient has a high likelihood of being a “technical success, but clinical failure” relative to the proposed spine surgery, at this time. In these cases, the patient may achieve a technical success as evidenced by perfect placement of the instrumentation and a solid fusion (or perfect placement of the ADR), but continue to report either no change in her symptoms or a worsening of her functional status. The biopsychosocial risk factors identified at this time, and reviewed previously, predict that Ms. Smith would not show any type of pain relief or functional improvement as a result of spine surgery. Therefore, the patient is not cleared for a spine surgery from a psychosocial perspective.
Risk of Psychiatric Decompensation. This assessment answers the question: Is the patient at significant risk for psychiatric decompensation as a result of proceeding with an elective spine surgery?
Aside from psychosocial factors predicting a poor clinical outcome, there is also a significant risk of psychiatric decompensation if this patient proceeds with the proposed elective spine surgery. The patient was found to be quite psychologically vulnerable as evidenced by the clinical history, mental status examination, and psychological testing. The patient was tearful during parts of the interview and experienced a panic attack while discussing her anxiety and depression. The patient has problems with impulse control as documented previously. She has just started seeing a counselor and has not yet been seen by a psychiatrist since being discharged from the hospital. All of these factors make her quite vulnerable to a psychiatric decompensation in response to a major spine surgery, especially if it is unsuccessful in relieving her pain or actually worsens her condition (which the psychosocial factors predict will occur as discussed previously). Therefore, from a biopsychosocial perspective, the patient is not cleared to undergo the elective spine surgery due to the high risk of psychiatric decompensation.
Alternative treatment with a better risk-Benefit Ratio: In cases where a patient is found to be a poor candidate for spine surgery, it is certainly reasonable to offer alternative treatments that have a chance for success. In these cases, I will often suggest that a comprehensive multi-disciplinary pain program be considered. This recommendation is consistent with the evidenced-based research and ACOEM and ODG Practice Guidelines. In the case of this patient, I do not believe that a full comprehensive multi-disciplinary pain program is necessary. I also do not believe that the patient would choose to pursue this type of treatment even if it were offered. However, I do believe there is another quasi-multidisciplinary intervention that does have a reasonable chance for success from a clinical and functional standpoint. In essence, this would include creating a multi-disciplinary intervention without the need for a formal program. The components of this intervention would be as follows:
Physical Reactivation: One of the hallmarks of a comprehensive multi-disciplinary pain program is physical reactivation and reconditioning. The results of the MPI and clinical interview suggest the patient is showing a very significant physical deconditioning and deactivation syndrome. In all likelihood, this is being facilitated by a fear of movement (kinesophobia) and fear of pain. Most pain and functional restoration programs will use a quota-based system for gradually increasing a patient’s level of function and strength.
It is interesting that the patient commented during the clinical interview that the only intervention that has provided any significant benefit has been a supervised exercise and strengthening program done near her home under the direction of Dr. Lami. She stated that the strengthening program helped with her pain, level of function, depression, and anxiety. As such, consideration might be given for allowing the patient to pursue functional restoration physical therapy treatment near her home on a three time per week basis. A typical course of this type of treatment might be 8-12 weeks with continued participation in treatment contingent upon objective gains. Given that this intervention has been useful in the past for this patient, it should have a fairly high likelihood of success. Assuming she successfully completes this intervention, consideration might also be given for a gym membership if it is felt that she is safe to exercise on her own. In appropriately motivated and carefully selected patients, this can certainly be a very cost effective and valuable intervention over the long term.
Psychological and Cognitive Behavioral Treatment: The patient is currently treating with a marriage and family therapist, Richard Jung, MA, MFT. I noticed on his business card that he specializes in addictions, clinical hypnotherapy, and pain management. The patient appears to have developed a therapeutic alliance with Mr. Jung and is looking forward to continuing to treat with him. As such, his interventions might focus on the psychological pain management issues concomitant with the physical reactivation intervention. In this scenario, it will be important for him to review such things as the gate control theory of pain, the difference between pain and suffering, the concept of “hurt does not equal harm,” and coping skills related to chronic pain management. It will also be important for this patient to develop other interests and distractive activities that will enhance her overall quality of life.
Psychopharmacology Treatment: The patient stated she has her first meeting with a new psychiatrist in mid-April. Concomitant with the other multi-disciplinary interventions, she will need ongoing psychopharmacology treatment. Although I was not provided a copy with the psychiatric AME, I assume this was recommended since the patient is seeing a psychiatrist on an industrial basis. The psychopharmacology intervention will certainly focus on helping her with her depression and anxiety. In addition, there are a variety of medications that are helpful for both depression and neuropathic pain. This treatment is just now starting.
Medication Management: Clearly, this patient has a propensity towards substance abuse as discussed throughout this evaluation report. According to the new opioid treatment guidelines recently published jointly by the American Pain Society and American Academy of Pain Medicine (Chou et.al. 2009), this patient is certainly not a candidate for any type of long term opioid maintenance. Given her history, it would be most prudent to either completely wean her off any opioid medication or taper it to the lowest dose and frequency of use possible. Also, in terms of medication management, this patient should be placed on the fewest possible medications to provide benefit. Lastly, consistent with multi-disciplinary pain treatment principles, all medications should be managed by one physician if possible.
Thank you for the opportunity to evaluate this woman. I reserve the right to change my opinion if and when other data become available such as more detailed medical records, etc. This evaluation has been completed consistent with the Practice Guidelines and recent changes in the Labor Code (per SB899).
WILLIAM W. DEARDORFF, PH.D., ABPP
As can be seen in the evaluation, a modified multidisciplinary pain program was recommended. In other cases, a full and comprehensive pain program might be recommended when a patient is found to be a poor candidate for spine surgery. Recent research has documented that these programs can provide results that are equal to spinal fusion and superior outcomes in patients that are poor spine surgery candidates. It is beyond the scope of this course to review all of the recent research in this area, however, Table 17 shows an example recommendation I use in these cases.
CONCLUSION
As we have reviewed in this course, in appropriate cases, biopsychosocial screening can be essential in terms of spine surgery decision-making. The goal is to identify those patients who have a high risk for technical success but clinical failure. Each day, countless patients undergo spine surgery and a significant number are headed towards becoming Failed Spine Surgery Syndrome cases. The behavioral health clinician is in a unique position to work with the spine surgeon to manage these cases effectively including pre-operative screening, preparation for surgery, and assistance with post-operative care.
REFERENCES
Aalto et al. (2006). Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis. Spine, 31, E648-E663.
Anderson et al. (2006). Work status as a predictor of surgical outcome of discogenic low back pain. Spine, 31, 2510-2515.
Block, A.R., Gatchel, R.J., Deardorff, W.W. & Guyer, R.D. (2003). The Psychology of Spine Surgery. American Psychological Association: Washington D.C.
Block et al. (2001). The use of presurgical screening to predict the outcome of spine surgery. Spine Journal, 1, 274-282.
Block et al. (1996). Discographic pain report: Influence of psychologic factors. Spine, 21, 334-338.
Carnes et al. (2006). A systematic review of pain drawing literature: Should pain drawing be used for psychologic screening? Clinical Journal of Pain, 22, 449-457.
Carragee, E.J. (2001). Psychological screening in the surgical treatment of lumbar disc herniation. The Clinical Journal of Pain, 17, 215-219.
Carragee, E.J. and Don, A.S. (2010). Provocative testing (Discography)(pp.131-140). In F. M. Phillips and C. Lauryssen (Eds.), The Lumbar Intervertebral Disc. New York: New York.
Daubs et al. (2008). Clinical instinct vs. standardized questionnaire: The spine specialists ablity to detect psychological distress. The Spine Journal, 8 Supplemental, 1S.
Deardorff, W.W. (2010). Presurgical psychological screening (pp. 142-147). In F. M. Phillips and C. Lauryssen (Eds.), The Lumbar Intervertebral Disc. New York: New York.
Deardorff, W.W. (2000). The MMPI-2 and chronic pain. In R.J. Gatchel and J.N Wiesberg (Eds.), Personality Characteristics of Pain Patients: Recent Advances and Future Directions. Washington, DC: APA Books.
DeBerard et al. (2001). Outcomes of posterolateral lumbar fusion in Utah patients receiving workers’ compensation. Spine, 26, 738-747.
Derby et al. (1999). The ability of pressure-controlled discography to predict surgical and nonsurgical outcomes. Spine, 24, 364-371.
Deyo, R.A. (2007). Back surgery – Who needs it? The New England Journal of Medicine, 356, 2239-2243.
Deyo, R.A. (2004). Spinal-fusion surgery: The case for restraint. The New England Journal of Medicine, 350, 722-726.
Dolan et al. (2000). Can exercise therapy improve the outcome of microdiscectomy? Spine, 12, 1523-1532.
Dubois et al. (2010). Decompressive surgery for herniated nucleus pulposus (open, micro, and minimally invasive approaches) (pp. 104-112). In F. M. Phillips and C. Lauryssen (Eds.), The Lumbar Intervertebral Disc. New York: New York.
Gatchel, R.J. and Turk, D.C. (1999). Psychosocial Factors in Pain: Critical Perspectives. New York: The Guilford Press.
Glassman, S.D., Anagnost, S.C. et al. (2000). The effect of cigarette smoking and smoking cessation on spinal fusion. Spine, 25, 2608-2615.
Glassman, S.D., Dimar, J.R. et al. (2007). The efficacy of rhBMP-2 for posterolateral lumbar fusion in smokers. Spine, 32, 1693-1698.
Hagg et al. (2003). Pain drawing does not predict the outcome of fusion surgery for chronic low-back pain: a report from the Swedish Lumbar Spine Study. European Spine Journal, 12, 2-11.
Ho, M.K. and Tyndale, R.F. (2007). Overview of the pharmacogenomics of cigarette smoking. The Pharmacogenomics Journal, 7, 81-98.
Hobby et al. (2001). The Distress and Risk Assessment Method (DRAM): Failure to predict the outcome of lumbar discectomy. The Journal of Bone and Joint Surgery, 83, 19-21.
Hutchins, T. and Maya, M. (2010). Degenerative disc imaging (pp. 126-130). In F. M. Phillips and C. Lauryssen (Eds.), The Lumbar Intervertebral Disc. New York: New York.
Kendrick et al. (2001). Radiography of te lumbar spine in primary care patients with low back pain: randomized controlled trial. British Medical Journal, 322, 400-405.
LaCaille et al. (2007). Obesity and litigation predict workers compensation costs associated with interbody cage lumbar fusion. The Spine Journal, 7, 266-272.
LaCaille et al. (2005). Presurgical biopsychosocial factors predict multidimensional patient outcomes of interbody cage lumbar fusion. The Spine Journal, 5, 71-78.
Luo et al. (2004). Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine, 29, 79-86.
Lurie, J.D. (2005). What diagnostic tests are useful for low back pain? Best Practice & Research in Clinical Rheumatology, 19, 557-575.
Main et al. (1992). The Distress Risk and Assessment Method: A simple patient classification to identify distress and evaluate the risk of poor outcome. Spine, 17, 42-52.
Manchikanti et al. (2009). Systematic review of lumbar discography as a diagnostic test for chronic low back pain. Pain Physician, 12, 541-559.
Mannion, A.F. and Elfering, A. (2005). Predictors of surgical outcome and their assessment. European Spine Journal, 155 Supplement, S93-S108.
Ohnmeiss et al. (1995). The association between pain drawings and CT/discographic pain responses. Spine, 20, 729-733.
Patel et al. (2007). Obesity and spine surgery: relation to perioperative comlcations. Journal of Neurosurgery Spine, 6, 291-297.
Patkar, A.A., Vergare, M.J. et al. (2003). Tobacco smoking: Current concepts in etiology and treatment. Psychiatry, 66, 183-199.
Ranny, L., Melvin, C. et al. (2006). Systematic review: Smoking cessation interventions strategies for adults and adults in special populations. Annals of Internal Medicine, 145, 845-856.
Spratt et al. (2004). A predictive model for outcome after conservative decompression surgery for lumbar spinal stenosis. European Spine Journal, 13, 14-21.
Stojanovic et al. (2007). Psychophysiological measurements during lumbar discography: A hear rate response study. Journal of Spine Disorders Techology, 20, 387-391.
Tandon et al. (1999). Posterior lumbar interbody fusion: Association between disability and psychological disturbance in noncompensation patients. Spine, 24, 1833-1838.
Trief et al. (2006). Emotional health predicts pain and function after fusion: A prospective multicenter study. Spine, 31, 823-830.
Trief et al. (2000). A prospective study of psychological predictors of lumbar surgery outcome. Spine, 25, 2616-2621.
Turner J.A. et al. (1992). Patient outcomes after lumbar spinal fusions. Journal of the American Medical Association, 268, 907-911.
Waddell, G. (1998). The Back Pain Revolution. London: Churchill Livingstone
Walsh et al. (1990). Lumbar discography in normal subjects. A controlled, prospective study. Journal of Bone and Joint Surgery, 72, 1081-1088.
Wolfer et al. (2008). Systematic review of lumbar provocation discography in asymptomatic subjects with a meta-analysis of false-positive rates. Pain Physician, 11, 513-538.
Zahrai, F. (1994). Microlumbar diskectomy: Is it safe as an outpatient procedure? Spine, 20, 1070-1074.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
PLEASE LOG IN TO VIEW OR TAKE THIS TEST
This test is only active if you are successfully logged in.










 in a recent review (Carnes et al., 2006). The pain drawing has been investigated as a predictor variable for spine surgery outcome but the results are inconsistent (Hagg et al., 2003). Even so, the pain drawing is easily administered and, when it is grossly abnormal, it is a useful piece of information to incorporate with other screening variables. Certainly, the pain drawing can be used adjunctively, but not as a stand-alone predictive test. The following pain drawings are clearly abnormal (Please see further discussion of pain drawings in the
in a recent review (Carnes et al., 2006). The pain drawing has been investigated as a predictor variable for spine surgery outcome but the results are inconsistent (Hagg et al., 2003). Even so, the pain drawing is easily administered and, when it is grossly abnormal, it is a useful piece of information to incorporate with other screening variables. Certainly, the pain drawing can be used adjunctively, but not as a stand-alone predictive test. The following pain drawings are clearly abnormal (Please see further discussion of pain drawings in the 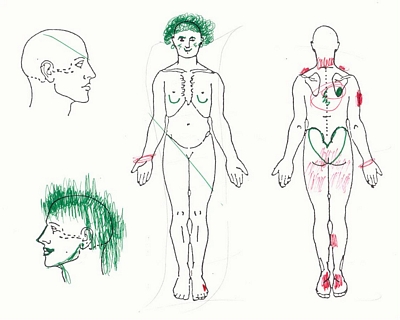 explain this pattern of pain. The possibility of a conversion disorder was considered.
explain this pattern of pain. The possibility of a conversion disorder was considered. referred him for routine screening. The patient was ultimately hospitalized on a psychiatric basis and began appropriate treatment after receiving a diagnosis of schizophrenia. Although he did have some objective findings relative to the pain symptoms, there was symptom amplification due to the psychological issues and spine surgery was determined not to be indicated. I think this case also underscores that, although the pain practitioner will primarily be involved with more behavioral health related issues, it is important for the clinician to be able to assess and appropriately manage these types of unusual psychiatric situations.
referred him for routine screening. The patient was ultimately hospitalized on a psychiatric basis and began appropriate treatment after receiving a diagnosis of schizophrenia. Although he did have some objective findings relative to the pain symptoms, there was symptom amplification due to the psychological issues and spine surgery was determined not to be indicated. I think this case also underscores that, although the pain practitioner will primarily be involved with more behavioral health related issues, it is important for the clinician to be able to assess and appropriately manage these types of unusual psychiatric situations.

